A new approach for bolstering the ability of T cells to fight cancer
A collaborative study led by the Monash Biomedicine Discovery Institute (BDI) has discovered a new immune checkpoint that may be exploited for cancer therapy.
The study shows that by inhibiting the protein tyrosine phosphatase PTP1B in T cells, the body’s immune response to cancer can be mobilized, helping to repress tumor growth.
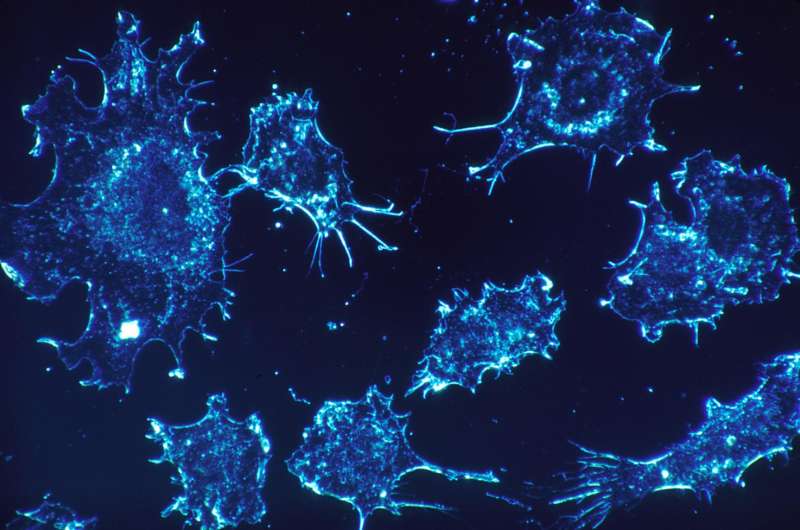
T cells are an essential part of the body’s immune system, helping not only to kill invading pathogens, such as viruses but also cancer cells. However, this study has shown that using a new drug candidate, the abundance of PTP1B in T cells that infiltrate tumors is increased, thereby restraining the ability of T cells to attack tumor cells and combat cancer. These findings have identified PTP1B as an intracellular brake, or checkpoint, reminiscent of the cell surface checkpoint PD-1—the blockade of which has revolutionized cancer therapy.
The findings are published in the prestigious journal Cancer Discovery.
Using mice, scientists from Monash BDI, in conjunction with colleagues at the Peter MacCallum Cancer Center in Melbourne and Cold Spring Harbor Laboratory in New York, found that by inhibiting PTP1B, using an early-stage injectable drug candidate that has previously been shown to be safe and well-tolerated in humans, the cancer-fighting ability of T cells is enhanced, repressing tumor growth.
Remarkably, the authors showed that the inhibition of this intracellular checkpoint, PTP1B, can also enhance the response to a widely used cancer therapy that blocks the PD-1 checkpoint on the surface of T cells.
Senior author Professor Tony Tiganis says that although the blockade of PD-1 can be highly effective against many tumors, not all patients respond and the development of resistance is common. This is true even for immunotherapy-sensitive cancers, such as melanoma. Approaches that can enhance the effectiveness or extend the utility of PD-1 checkpoint blockade are highly sought after in the clinic.
“While more pre-clinical work is needed, our findings show that superior outcomes were achieved when we combined PTP1B inhibition with existing immunotherapies in mice,” said Professor Tiganis.
In addition, beyond enhancing the response to PD-1 blockade, the authors showed that the inhibition of PTP1B also significantly enhanced the effectiveness of cellular therapies using Chimeric Antigen Receptor (CAR) T cells.
CAR T cells are T cells derived from a patient’s blood that are modified in the lab so that they produce a man-made receptor to help them better identify tumor cells and then injected back into the patient.
CAR T cells have been highly effective against some blood cancers; however, this success has not, as yet, been replicated in solid tumors. The authors demonstrate that the deletion or inhibition of PTP1B can dramatically enhance the ability of CAR T cells to attack solid tumors in mice, including breast cancer.
“To advance this work, a key next step will be to further define the impact of PTP1B deletion in CAR T and conventional T cells in humans. There remains an urgent clinical need to identify and validate cellular targets to revive and sustain T cell responses in cancer,” said first author Dr. Florian Wiede.
Professor Tiganis and Dr. Wiede will also continue to collaborate with Cold Spring Harbor Laboratory and DepYmed Inc., a US-based company developing PTP1B inhibitors, to test in their preclinical models orally bioavailable PTP1B inhibitor drug candidates as novel checkpoint inhibitors. These findings could form the basis of future clinical trials.
Cancer continues to be a major cause of illness and death in Australia, accounting for 30 percent of all deaths in Australia in 2020. The AIHW cancer in Australia report estimates that around 185,000 cases of cancer will be diagnosed in 2031 and that between 2022 and 2031, a total of around 1.7 million cases of cancer will be diagnosed.
Source: Read Full Article
