ALS treatment: FDA to rule on drug toferson for type of the disease

- More than 200,000 people around the world have ALS.
- There is currently no cure for the disease and most people die within three to five years from diagnosis.
- As much as 20% of ALS cases are caused by a mutation in the SOD1 gene.
- The U.S. FDA is evaluating a new drug called tofersen for people with SOD1-ALS and is expected to decide on the medication ruling on April 25.
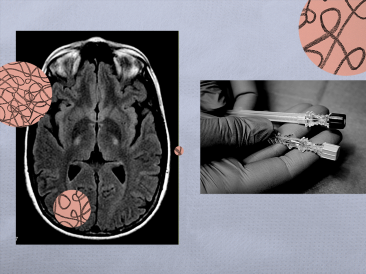
More than 200,000 people globally have amyotrophic lateral sclerosis (ALS) — a progressive disease of the nervous system that affects the nerve cells in the brain and spinal cord.
There is currently no cure for ALS. Most people with the disease die within three to five years of diagnosis from respiratory failure. About 10% of people with ALS live for another 10-plus years.
In an effort to add to treatments available for ALS, pharmaceutical company Biogen is currently waiting to see if the U.S. Food and Drug Administration will approve its investigational antisense drug tofersen for people with superoxide dismutase 1 (SOD1) ALS.
The FDA is expected to issue its ruling on April 25, 2023.
What is ALS?
ALS specifically targets a type of nerve cell called motor neurons.
As the motor neurons diminish, the nervous system is no longer able to send messages to the muscles, causing them to weaken and stop working.
Signs and symptoms of ALS include:
- weakness in the hands, legs, ankles, and feet
- inability to maintain good posture
- difficulty walking
- muscle twitches or cramps
- slurred speech
- difficulty eating or swallowing
As the disease progresses, people with ALS will eventually not be able to stand or walk unaided. They will also be unable to use their hands and arms.
People with ALS may also experience difficulty speaking, eating, and breathing.
Risk factors for ALS include:
- Age — Although the disease can strike at any age, symptoms commonly develop between the ages of 55 and 75
- Gender — Men are more likely to develop ALS.
- Ethnicity — ALS affects people from all races and ethnic backgrounds but is more commonly seen in Caucasians and non-Hispanics.
The majority of ALS cases are considered sporadic, meaning they occur in people without a family history of the disease.
About 10% of ALS cases are considered familial, meaning the disease was inherited.
What is SOD1-ALS?
Genetics plays a role in many familial ALS cases.
For example, a defect in the C9ORF72 gene is responsible for about 40% of familial ALS cases.
A mutation of the SOD1 gene accounts for between 10% to 20% of all familial ALS.
The SOD1 gene is responsible for making an enzyme that binds to copper and zinc molecules in the body, allowing it to break down toxic molecules called superoxide radicals.
According to Dr. Toby Ferguson, the vice president and head of the Neuromuscular Development Unit at Biogen, SOD1-ALS is a rare genetic form of ALS diagnosed in approximately 330 people in the United States.
“It can advance quickly, is always fatal, and can have a devastating impact on families for generations,” he told Medical News Today. “If approved, tofersen would represent a new scientific advance for the ALS community as the first and only treatment to target a genetic cause of ALS. We hope this will pave the way for further advances in this relentless disease.”
How does tofersen work?
Ferguson said tofersen is an antisense oligonucleotide (ASO) being evaluated for the treatment of SOD1-ALS.
“ASOs are short, synthetic strings of nucleotides designed to selectively bind to target RNA and regulate gene expression,” he explained. “In people with SOD1-ALS, mutations in their SOD1 gene cause their bodies to create a toxic form of SOD1 protein. This toxic form of SOD1 protein causes motor neurons to degenerate, resulting in progressive muscle weakness.”
“Tofersen is designed to bind and degrade SOD1 mRNA in an effort to reduce the production of SOD1 protein,” Ferguson added.
Phase 3 results
Ferguson said the integrated 12-month data from the phase 3 VALOR clinical trial and its open-label extension (OLE) have shown reductions in neurofilament — a marker of damage to neurons and neurodegeneration.
“These are critical measures for people living with this devastating disease,” he said. “In addition, tofersen lowered levels of neurofilament — a marker of axonal injury and neurodegeneration — in patients by approximately 40 to 50 percent.”
“There is extensive literature indicating that neurofilament levels are prognostic for disease progression and survival, with higher levels associated with (a) more rapid decline in clinical function and shortened survival,” Ferguson added. “The combination of these biomarker results and the clinical outcomes data provide additional evidence of tofersen’s potential to effectively slow the progression of SOD1-ALS.”
Biogen states in their press release that tofersen did not meet the primary endpoint of change from baseline to week 28 in the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R). However, researchers did find tofersen led to less decline in motor function, respiratory function, muscle strength, and quality of life in people with SOD1-ALS.
Awaiting FDA ruling
Tofersen is currently under review by the FDA.
Those regulators were originally expected to vote on its approval on January 25. The approval date was then moved to April 25.
On March 22, the U.S. Food and Drug Administration’s (FDA) Peripheral and Central Nervous System Drugs Advisory Committee provided its own evaluation of the effectiveness of tofersen.
According to a press release from Biogen, the advisory committee declared the effectiveness of the experimental drug wasn’t sufficient.
However, the advisory committee did state that tofersen’s ability to reduce in-plasma neurofilament light chain (NfL) concentration is “reasonably likely” to provide clinical benefit to people with SOD1-ALS.
“This is a monumental step forward for the ALS field in which objective measures sensitive to treatment-driven changes, particularly earlier in the disease course, are in high demand,” Ferguson said. “We find ourselves here in large part because of the work the ALS community has done to characterize the behavior of neurofilament over the past decade.”
“While the appropriateness of neurofilament as a potential surrogate will be evaluated on a case-by-case basis, we hope the data from the tofersen program will be an additional catalyst for the use of neurofilament and other novel biomarkers in the future,” he added.
Hopeful clinical benefit
Dr. Santosh Kesari, a neurologist at Providence Saint John’s Health Center in California and the regional medical director for the Research Clinical Institute of Providence Southern California, told Medical News Today his hope for tofersen is that it will improve survival and reduce the progression of the disease and maintain a higher quality of life for patients with ALS.
“It’s an interesting class of drugs that is based on the modifying DNA expression of the SOD1 gene,” he explained. “Tofersen inhibits the expression of SOD1 mutation, which we think causes the ALS symptoms in the less common genetic subtype of ALS caused by SOD1 mutations.”
“There are many studies over the years showing if you knock down or suppress the mutant SOD1, you can rescue or preserve the function of those neurons,” Kesari continued. “And this drug is basically targeting the mutant gene and suppressing its expression in preventing the pathology of ALS and the neurotoxicity inflammation and decline of those neurons that results in ALS symptoms.”
Kesari mentioned the tofersen Phase 3 VALOR study did not meet its primary or secondary endpoints since the trial length of 28 weeks was short and may not have been enough time to observe tofersen’s effect on disease progression.
“But there was clearly a reduction in surrogate markers of SOD1 protein expression being reduced,” he said. “And more intriguingly, they found that NfL — a general marker of neuronal damage — was 55 percent lower at 28 weeks in the tofersen group compared to a 12 percent increase in the placebo group, suggesting that tofersen treatment may have an effect in preventing neurodegeneration and may have a clinical benefit.”
Future potential
Medical News Today also spoke with Dr. Jeffrey D. Rothstein, a professor of neurology and neuroscience and director of the Robert Packard Center for ALS Research at Johns Hopkins University School of Medicine in Maryland, about tofersen and the upcoming FDA announcement.
“It’s a uniformly fatal disease, so any drug that can slow the disease down is obviously important,” he said. “Some SOD1 mutations progress in nine months from the first symptoms to the time the patient dies, so any drug therapy that can slow it down is great. This is targeted specifically for those patients who carry that mutation — it is not applicable to patients who have just sporadic ALS.”
Rothstein added that approval of a gene therapy such as tofersen may open the door for treatments to be used in pre-symptomatic patients.
“Say you know your family has ALS — you can get tested (and) you know you carry the SOD1 gene,” he explained. “There is now a clinical trial where we’re treating patients before they get the disease. If you give a drug to someone who has a gene defect before they actually show disease, where you stop the disease ever from showing up or substantially slow its onset or progression… that’s the ultimate medicine, truly preventative medicine. And so this first approval heralds that next step.”
Source: Read Full Article