Aortic stenosis: TAVR procedure more effective than open-heart surgery

- Aortic stenosis, which involves the narrowing of the aortic valve that controls blood flow from the heart to the aorta, can lead to life-threatening complications such as heart attacks and stroke.
- Open heart surgery has been conventionally used for the treatment of severe aortic stenosis, but transcatheter aortic valve replacement (TAVR), a minimally-invasive procedure, is now preferred for people who are at high risk of death or complications due to invasive surgery.
- Federal regulators have approved TAVR for the treatment of aortic stenosis patients at low surgical risk, but there is a lack of data on the long-term outcomes of this procedure.
- A new study shows that TAVR was associated with a lower risk of death, stroke, and rehospitalization but an increased risk of needing a pacemaker than open-heart surgery during the three-year follow-up period.
A recent study published in the Journal of the American College of Cardiology suggests that minimally invasive transcatheter aortic valve replacement (TARV) procedures led to durable superior clinical outcomes compared with open heart surgery over a 3-year follow-up period.
The researchers report that TARV led to a greater decline in the incidence of all-cause mortality and stroke as well as better performance of the replacement valve after the procedure, compared with open heart surgery.
“This study shows that the initial benefit of TAVR remained broadly consistent over the first three years,” said Dr. John Forrest, the first author of the study and an associate professor of medicine at Yale University in Connecticut, in a statement. “In patients who are at low risk for death, stroke, or other serious complications of aortic valve surgery, we need to have compelling evidence that TAVR is both safe and effective and also that the results are durable. The consistent benefit of TAVR at three years is not something that has been observed in prior studies and provides further evidence that TAVR deserves to be the dominant treatment modality for patients with aortic stenosis undergoing valve replacement.”
Dr. Sanjiv Patel, an interventional cardiologist at MemorialCare Heart & Vascular Institute at Orange Coast Medical Center in California who was not involved with the study, said the findings are important.
“The most significant aspect of this study is that it looked at the low-risk patient for TAVR and its outcome,” Patel told Medical News Today. “The study showed that TAVR was more effective than open-heart surgery with regard to mortality and stroke three years after the new valve implantation. It also demonstrated that TAVR had a higher pacemaker rate than open-heart surgery, which further validated what we clinically already recognize to be true.”
Aortic stenosis treatment options
The aortic valve is located between the lower left chamber of the heart and the aorta, the largest artery providing oxygenated blood to the body. The aortic valve regulates blood flow between the left ventricle of the heart and the aorta.
Aortic stenosis is one of the most common valve diseases, found in 5% of individuals aged over 65 years of age. Aortic stenosis is characterized by the narrowing of the aortic valve, reducing the supply of blood from the left ventricle to the aorta.
Common symptoms of aortic stenosis include chest pain, shortness of breath, rapid or irregular heartbeat, and fatigue.
The narrowing of the aortic valve causes the heart to work harder and leads to a compensatory thickening of the left ventricle wall. The thickening of the left ventricle walls, known as left ventricular hypertrophy, can lead to complications such as heart failure, cardiac arrest, and stroke.
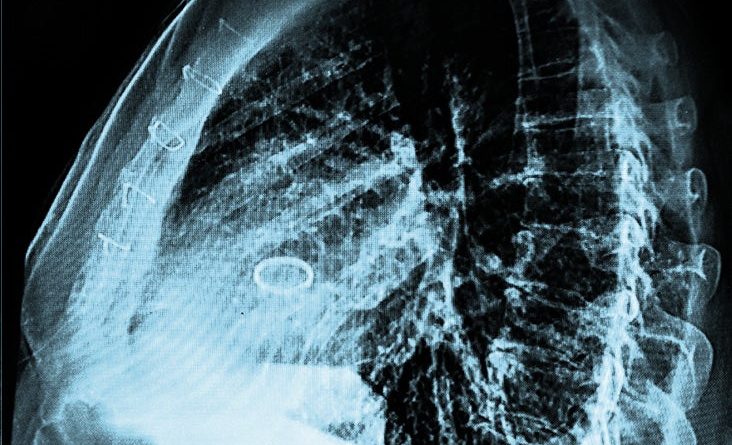
Severe aortic stenosis requires the replacement of the faulty aortic valve. Invasive open-heart surgery involving an incision to access the heart has traditionally been used to replace the faulty aortic valve.
During open-heart surgery, also known as surgical aortic valve replacement, the faulty aortic valve is replaced with a new valve made of synthetic materials or derived from pig, cow, or human heart tissue.
What to know about TAVR procedures
More recently, transcatheter aortic valve replacement (TAVR), a minimally-invasive procedure, has emerged as an alternative to surgical aortic valve replacement.
In TAVR, the old valve is not replaced. Instead, a new valve is placed inside the defective valve with the help of a flexible, thin tube or catheter. The catheter is generally inserted through a small incision in the leg into an artery to deliver the replacement valve to the heart.
TAVR has supplanted surgical aortic valve replacement (SAVR) in high-risk patients who cannot withstand invasive surgery due to the risk of complications or mortality.
Previous studies have shown that TAVR is associated with lower mortality in high-risk patients than SAVR. Similarly, studies in patients at intermediate surgical risk have shown that TAVR produces similar or superior clinical outcomes than open-heart surgery.
The Federal Drug Administration approved the use of TAVR in individuals under 75 years of age with severe aortic stenosis. However, there is only short-term data available comparing outcomes after TAVR with SAVR in patients at low-surgical risks.
The major concerns with the use of TAVR include the long-term durability of the valve and the potential of paravalvular regurgitation or leak. A paravalvular leak refers to blood leaking back into the left ventricle due to inadequate sealing between the replacement valve and the natural heart tissue.
The present study was conducted as a part of the Evolut LowRisk trial to assess the long-term outcomes in aortic stenosis patients undergoing TAVR.
Impact of TAVR
The current study consisted of 1,414 participants with severe aortal stenosis randomly assigned to receive either TAVR or open-heart surgery. The average age of the study’s participants was 74 years.
To compare the clinical outcomes in patients undergoing TAVR or surgery, the researchers assessed the incidence of all-cause mortality or disabling stroke during the three-year follow-up period.
They also examined the performance of the replacement valve using echocardiography, a type of ultrasound scan used to examine the function of the heart and blood vessels.
The incidence of all-cause mortality or disabling stroke was lower in patients undergoing TVAR (7%) than in the open-heart surgery group (10%) during the three-year follow-up period. These differences in the incidence of all-cause mortality and disabling stroke were consistently observed at the end of 12, 24, and 36 months
The patients in the TAVR also show lower rates of atrial fibrillation, a type of irregular heartbeat that originates in the heart’s upper chamber.
During aortic valve replacement surgery, the size of the orifice of the prosthetic valve can sometimes be smaller than necessary for adequately supplying blood to the body and can result in the worsening of symptoms. This phenomenon is referred to as prosthesis-patient mismatch.
Studies have shown that prosthesis-patient mismatch is associated with an increased risk of structural deterioration of the valve and mortality.
In the current study, there were more than twice as many cases of moderate-to-severe prosthesis-patient mismatch in individuals who underwent open-heart surgery (25%) than in those that underwent TAVR (10%).
Echocardiography also revealed a greater improvement in the functioning of the aortic valve after TAVR than open-heart surgery. Both groups showed improvements in life quality, but these improvements were more rapid in the group that underwent TAVR.
A previous study showed that moderate-to-high paravalvular leakage after TAVR is associated with higher rates of mortality 5 years after the intervention. In the current study, the rates of moderate and high paravalvular regurgitation were similar in patients in the TAVR and open-heart surgery groups.
However, mild paravalvular leakage or regurgitation was more commonly observed in participants who underwent TVAR (20%) than open-heart surgery (2%). Individuals with mild paravalvular leakage at 30 days were not at a higher risk of mortality or disabling stroke by the end of the follow-up period.
Controlling the heartbeat
The conduction system of the heart contains specialized muscle cells that transmit electrical impulses through the heart and cause contraction of the heart chambers, thus controlling the heartbeat.
The placement of the valve during TAVR can cause damage to the heart’s conduction system, with patients often requiring a new pacemaker after TAVR.
Consistent with this, the number of individuals requiring pacemaker placement was higher in the TAVR group (23%) than in the surgery group (9%). The mortality rate was higher in patients who had a pacemaker implanted within 30 days after TAVR than those who did not need a pacemaker.
The type of prosthetic valves used for TAVR in the study could also limit access to coronary arteries that supply blood to the heart muscle. This could hinder the treatment of coronary artery disease.
“Coronary access may be more difficult with TAVR with supra-annular valves, and while it did not affect 3-year mortality, it may become an issue during longer-term follow-up,” Dr. Michael Broukhim, an interventional cardiologist at Providence Saint John’s Health Center in California, who was not involved in the study, told Medical News Today.
“The researchers intend to follow the patients for a total duration of 10 years to fully understand the long-term risks and benefits after TAVR,” he added. “The significance of this study is that 3-year outcomes seem to be comparable between TAVR and surgical aortic valve replacement. Longer-term follow-up data will be important to evaluate which treatment will be best for low-risk patients due to the importance of long-term durability and potential valve reintervention rates.”
Dr. Nish Harshadkumar Patel, an interventional cardiologist at Miami Cardiac and Vascular Institute, part of Baptist Health South Florida, who was also not involved in the study, told Medical News Today that “physicians can consider this finding when educating the patients and engaging in shared decision-making regarding the choice between the TAVR and surgery for the aortic valve replacement in low-risk patients.”
Source: Read Full Article