BNT162b2 mRNA COVID-19 vaccine-induced antibodies wane over six month period
As vaccination programs around the globe are beginning to slow, the transmission of coronavirus 2019 (COVID-19) has risen again, with concern rising over the spread of dangerous variants of concern (VOCs). These variants are known to evade immune responses effective against the original strain found in Wuhan, China. Of particular concern is the Delta variant, which arose in India to quickly become the most dominant strain worldwide, and the cause of most new cases.
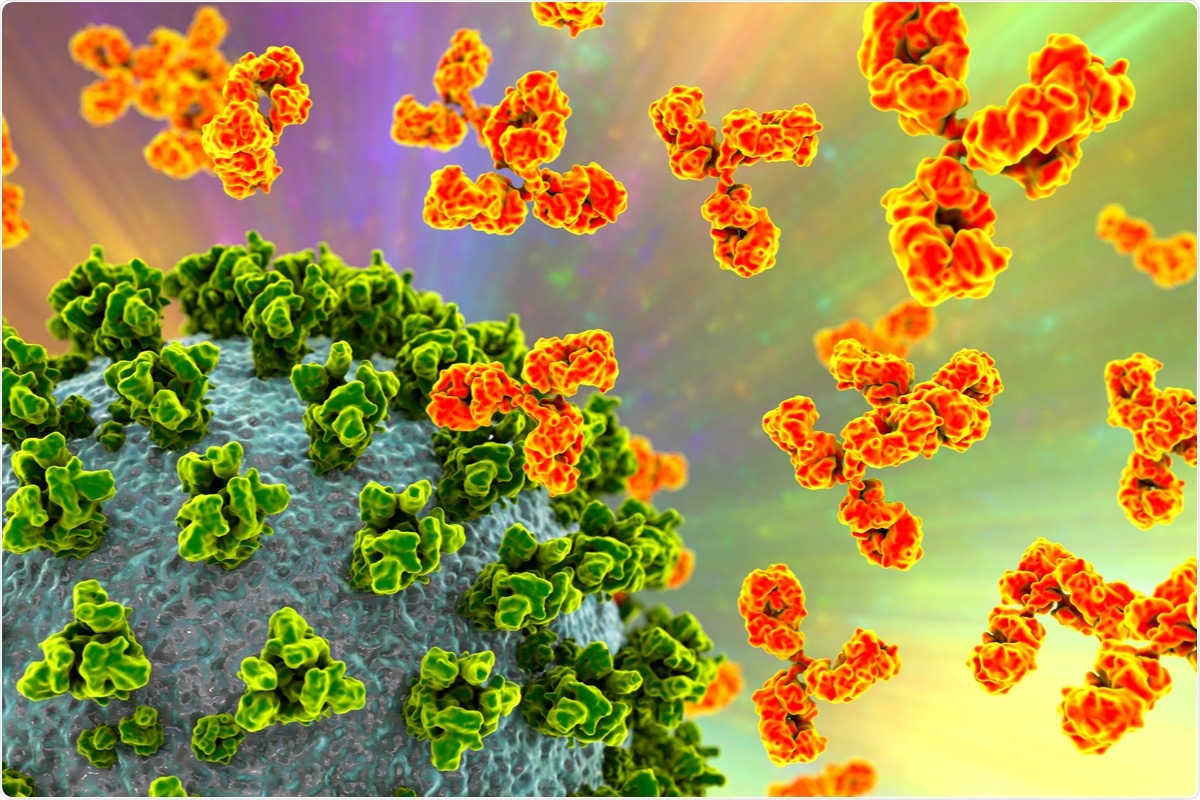
Most VOCs are created by mutations that affect the spike protein of severe acute respiratory syndrome coronavirus 2019 (SARS-CoV-2), especially the receptor-binding domain (RBD) of the S1 subunit, as this is the region that binds to angiotensin-converting enzyme 2 (ACE2), allowing membrane fusion and viral entry into the cell.
In particular, the mutations present in the VOCs alter the conformation of the three monomers that make up the spike protein trimer. In wild-type COVID-19, all three are normally in the down conformation, which helps evade the immune response. However, in the more infectious variants such as the Delta variant, one or more of the monomers tend to be in the up conformation, allowing greater binding to ACE2 and increased transmission.
Researchers from the Uniformed Services University in Bethesda have been investigating the response of antibodies created against SARS-CoV-2 by the Pfizer-BioNTech six months after vaccination, as well as the differing ability of these antibodies to combat VOCs. The Pfizer-BioNTech BNT162b2 is an mRNA vaccine that produces immunity by providing the cell with the mRNA for a protein, such as the SARS-CoV-2 spike protein.
The cellular machinery then translates this, producing the protein, and allowing the immune system to develop a response against it without any danger. As no viral structural proteins are involved, and as mRNA is non-infectious and non-integrating, it is safer than more traditional vaccines created from inactive strains of the virus, which can reactivate or cause allergic reactions.
A preprint version of the group's study is available on the medRxiv* server while the article undergoes peer review.
The study
The researchers enrolled healthy adult healthcare workers at the Walter Reed National Military Medical Center who presented with no anti-SARS-CoV-2 spike protein IgG antibodies, showed no history of COVID-19 into the study, and collected serum samples monthly. These samples were then screened for IgG reactivity against the spike and nucleocapsid proteins using multiplex microsphere-based immunoassays.
The ability of the serum samples to neutralize SARS-CoV-2 was determined using a lentiviral pseudovirus SARS-CoV-2 neutralization assay – this was used for both wild-type and the Delta variant. Individuals infected before January 21, 2021, were excluded from the study. In total, 227 vaccinated individuals and 17 non-vaccinated individuals were followed.
All vaccinated individuals showed seroconversion against SARS-CoV-2 when tested a month following the second vaccine dose. Anti-spike IgG bAb and nAb then slowly decreased over a six-month duration. At every point of the experiment, both bAbs and nAbs showed significantly higher binding and reactivity against wild-type SARS-CoV-2 compared to the Delta variant.
This is supported by multiple other studies showing reduced vaccine-induced immune response against the Delta variant compared to wild-type. Two vaccinated patients were found to have a symptomatic infection with SARS-CoV-2 post-vaccination, both of which were mild cases that did not require hospitalization. Four non-vaccinated individuals contracted COVID-19, one of whom required ICU care.
Conclusion
The researchers highlight the value of their work in helping to inform vaccine manufacturers and public health policymakers of the responses seen in vaccinated individuals against SARS-CoV-2 wild-type and the Delta strain and how these responses can change over time. The authors point to the frequency of gathering serum samples and subsequent serological assessments, the use of variant-specific neutralizing antibodies, and the multiplexed antigen-specific IgG detection as factors that greatly increase the strength of the study's strength.
While similar studies have examined larger populations, the researcher's data and analyses could prove invaluable in helping to identify factors that could grow to become larger factors. This study shows that as many people as possible must become vaccinated – strains like the Delta variant capable of evading natural and vaccine-induced immunity continue to arise. With mass vaccination programs in both the United States and the United Kingdom beginning to stall, it could allow time for even more dangerous variants to arise.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Laing, ED. et al., (2021) Durability of antibody responses and frequency of clinical and subclinical SARS-CoV-2 infection six months after BNT162b2 COVID-19 vaccination in healthcare workers. medRxiv. doi: https://doi.org/10.1101/2021.10.16.21265087
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antigen, Assay, Cell, Coronavirus, Coronavirus Disease COVID-19, Enzyme, Frequency, Healthcare, Immune Response, Immune System, immunity, Immunoassays, Membrane, Protein, Pseudovirus, Public Health, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Sam Hancock
Sam completed his MSci in Genetics at the University of Nottingham in 2019, fuelled initially by an interest in genetic ageing. As part of his degree, he also investigated the role of rnh genes in originless replication in archaea.
Source: Read Full Article
