COVID-19 vaccination protects people with B cell lymphoma and multiple myeloma
People with hematologic malignancies are at greater risk of severe coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); however, studies exploring the immune response to the COVID-19 vaccine have been scarce. A recent Nature Cancer study documented that individuals with B cell lymphomas (LY) and multiple myeloma (MM) developed potent infection neutralization capabilities against several SARS-CoV-2 variants of concern (VoCs).
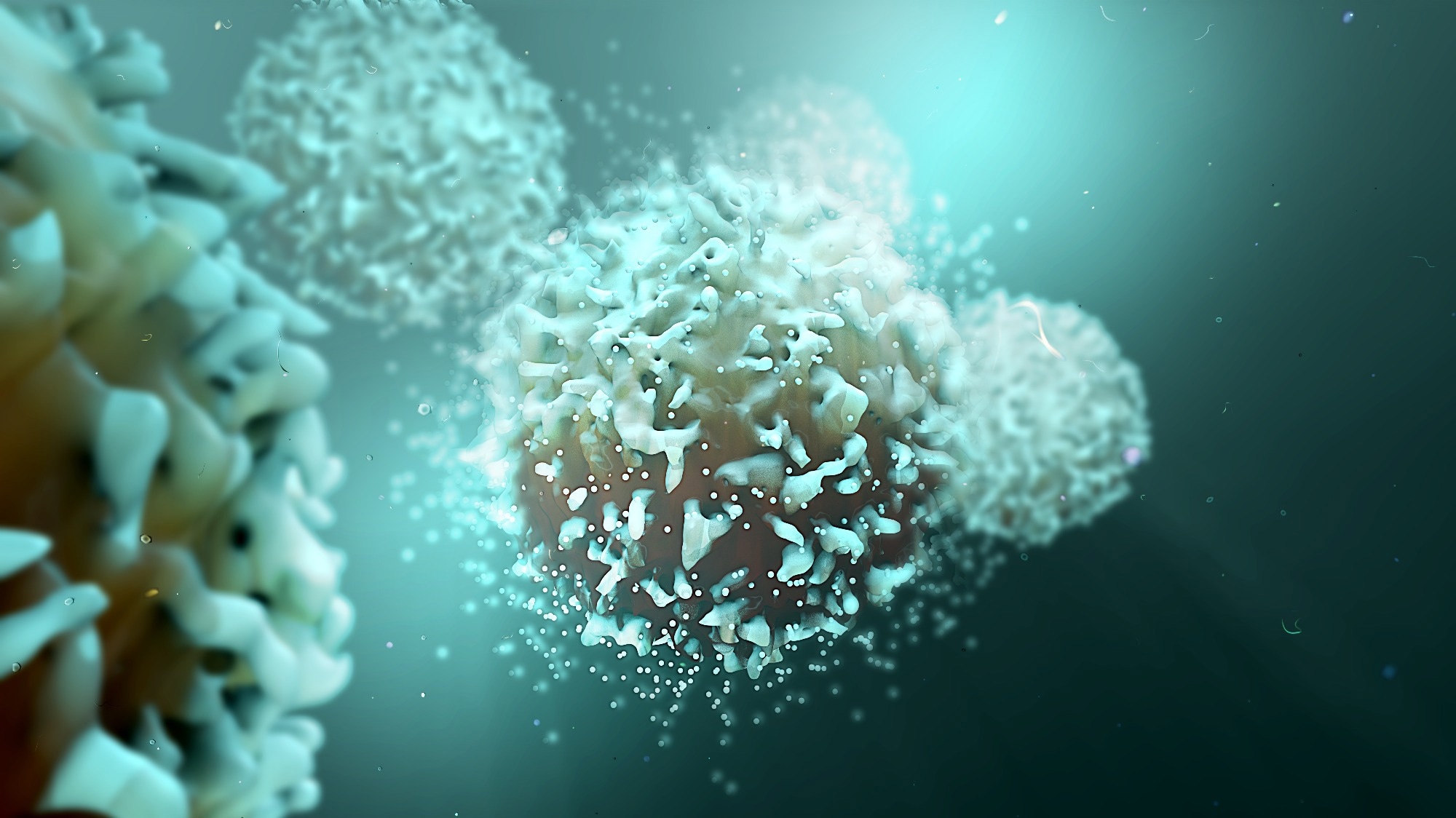 Study: Potent high-avidity neutralizing antibodies and T cell responses after COVID-19 vaccination in individuals with B cell lymphoma and multiple myeloma. Image Credit: Design_Cells / Shutterstock
Study: Potent high-avidity neutralizing antibodies and T cell responses after COVID-19 vaccination in individuals with B cell lymphoma and multiple myeloma. Image Credit: Design_Cells / Shutterstock
About the Study
Patients with cancer have shown high mortality and morbidity rates due to SARS-CoV-2 infection. Such individuals often have secondary immunodeficiency and contract severe disease. Studies have demonstrated the efficacy of available vaccines in reducing disease severity in immunocompetent individuals, inducing both T-cell and humoral responses.
The current study deployed a longitudinal approach to study the T cell and humoral immune responses generated by two and three vaccine doses, using mainly the BNT162b2 mRNA vaccine. The cohort of individuals had different B cell LYs and MM. Researchers were able to obtain a thorough picture of vaccine-induced immune responses in this group compared to a healthy control group. Parallel and time-resolved assessment of antibody titers to viral spike protein, neutralization capacity, and antibody avidity to six authentic, replication-competent viruses, and HCoV OC43- and SARS-CoV-2-directed T cell responses were analyzed.
Key Findings
Six key findings were reported in the current study. First, compared to healthy individuals, individuals with hematologic malignancy demonstrated only a slightly lower infection neutralization capacity against SARS-CoV-2 variants. This was despite much lower antibody titers to the spike protein in the treated group.
Second, the per anti-spike antibody unit neutralizing potency was drastically enhanced in individuals with hematologic malignancies (20.8 fold on average), compared to the control group. This enhancement was observed early after the second vaccination. Third, compared to healthy individuals, the treated group showed higher avidity of serum IgG binding to the viral spike protein ahead of receiving the third vaccine dose.
Immunology eBook
Fourth, the Omicron (BA.1) and, to a lesser extent, Beta and Delta VoCs showed the greatest humoral immune escape. This finding was consistent with recent results on healthy individuals post-vaccination or infection. Fifth, the dominant share of study participants mounted robust vaccine-induced T-cell responses to several recent VoCs. This group included those participants that had LY and were receiving Rx treatment. Sixth, no COVID-19-related death was reported in the study cohort and the clinical presentation during breakthrough infections proved that the vaccine offered partial protection in immunocompromised individuals with hematologic malignancies.
The results indicated that individuals with LY without a humoral immune response were at a greater risk of contracting symptomatic breakthrough infections. This highly immunosuppressed group could benefit from preexposure prophylaxis with neutralizing mAbs, although most currently available mAbs have shown a loss of antiviral efficacy for recent VoCs.
It was observed that the third vaccination was important in both groups to elevate antibody titers. However, it was proposed that the quality rather than the quantity of spike-targeting antibodies were of greater importance. The absolute quantity could, therefore, belittle the potency of the humoral response in vaccinees with MM or LY.
Research has shown that mRNA-based vaccines induce spike-specific T-cell responses in most healthy recipients. However, more heterogeneous responses have been reported in individuals with cancer. The results on vaccine-induced T cell responses, elicited by 85% of individuals with hematologic cancers included in the study, were consistent with those documented in a large British cancer-cohort study. In the latter study, the response rate in a cohort of individuals with hematologic cancers was 80%.
Strengths and Limitations of the Current Study
The key strength of the study is the longitudinal sampling of clinically well-characterized individuals with cancer and their subsequent matching with a group of healthy healthcare workers. The robust methodological approach, including quantifying anti-spike IgG avidity and live virus neutralization assays, is another strength of the current study.
The critical limitation of the study is the small number of individuals with hematologic cancer (N = 60). A contemporaneous control group concerning solid tumors or other hematologic malignancies was also absent. Additionally, no adjustments were made for multiple testing in correlation analysis, which may have introduced confounders.
Conclusions
More detailed longitudinal studies of COVID-19 immunity induced by infections and vaccines should use multiparametric assessment. This is crucial as we further our understanding of quantitative markers as correlates of protection in individuals with hematologic malignancies as new SARS-CoV-2 VoCs emerge.
- Keppler-Hafkemeyer, A., et al. (2022) Potent high-avidity neutralizing antibodies and T cell responses after COVID-19 vaccination in individuals with B cell lymphoma and multiple myeloma. Nature Cancer. https://doi.org/10.1038/s43018-022-00502-x, https://www.nature.com/articles/s43018-022-00502-x
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Antibodies, Antibody, B Cell, Cancer, Cell, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Healthcare, Immune Response, immunity, Immunodeficiency, Lymphoma, Mortality, Multiple Myeloma, Myeloma, Omicron, Prophylaxis, Protein, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, T-Cell, Vaccine, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
