Estimating gastric cancer risk using DNA methylation and lifestyle data
Gastric cancer is the fourth leading cause of cancer-related mortalities worldwide. Various environmental and lifestyle-related factors, like tobacco and alcohol consumption, are known to contribute to the risk of gastric cancer. Further, infection by Helicobacter pylori–a bacterium found in the stomach–is another leading risk factor for the onset of the disease.
H. pylori infection can cause inflammation and exacerbated aberrant DNA methylation in the stomach mucosa. Aberrant DNA methylation due to H. pylori infection can accumulate in the gastric mucosa years before the onset of gastric cancer. DNA methylation in the promoter region of tumor-suppressing genes is known to cause silencing of these genes and eventual carcinogenesis in the tissue.
However, it remains to be confirmed whether DNA methylation caused by H. pylori infection can be used as a marker for future gastric cancer. Further, there are no reports on how the interaction between DNA methylation and lifestyle factors influences the development of gastric cancer.
An international team of researchers, led by Prof. Atsushi Kaneda from Chiba University, Japan, with Prof. Patrick Tan, Senior Vice-Dean for Research & Professor, Cancer & Stem Cell Biology Signature Research Programme, Duke-NUS Medical School and Prof. Khay Guan Yeoh, Kishore Mahbubani Professor in Medicine and Health Policy from the Department of Medicine at the Yong Loo Lin School of Medicine, National University of Singapore, has recently demonstrated how DNA methylation and lifestyle factors interact and influence the risk of gastric tumor development, also known as gastric neoplasia (GN).
The study also involved Dr. Genki Usui and other researchers from the following institutions in Japan and Singapore: Chiba University, The University of Tokyo, NTT Medical Center Tokyo, Tokyo University of Science (all in Japan); and Duke-NUS Medical School, the Yong Loo Lin School of Medicine, National University of Singapore, National University Hospital, Tan Tock Seng Hospital, Singapore General Hospital, and Changi General Hospital (all in Singapore).
They collaborated on co-authoring the manuscript published in eBioMedicine. Discussing his motivation to pursue the research, Dr. Kaneda, who was formerly a gastrointestinal surgeon, says, “It is, of course, very important to cure patients who have already developed cancer, but I believe it would be more helpful if we can manage cancer risk before cancer development.”
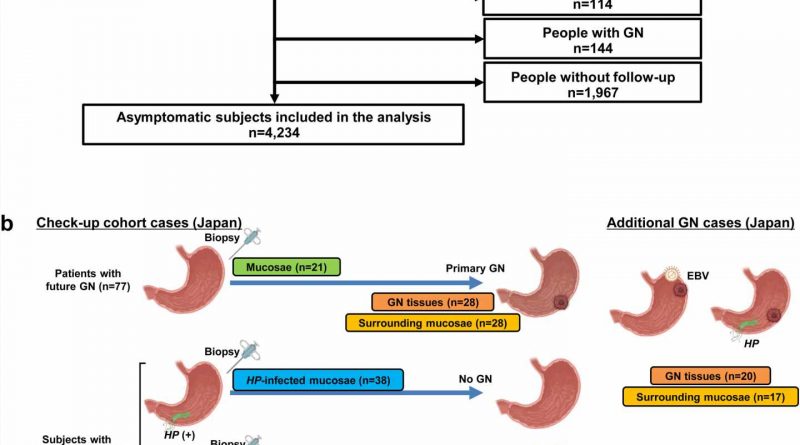
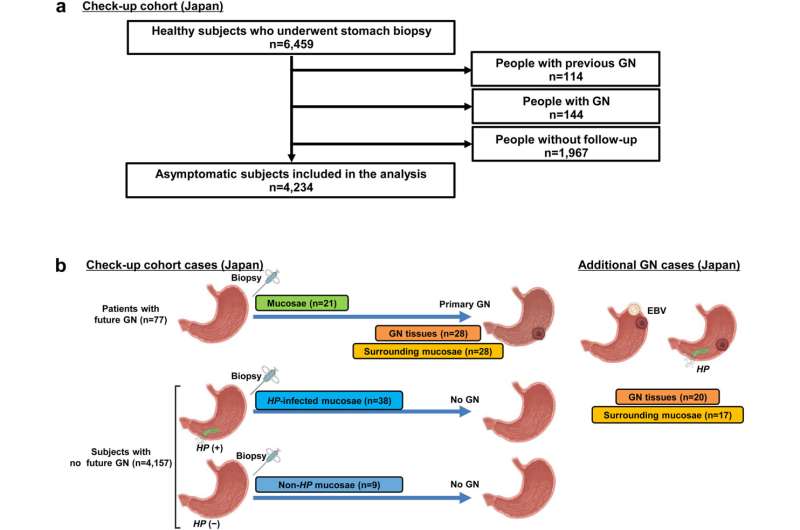
The team studied the association between clinical factors and GN development. They examined gastric mucosal biopsy samples collected from asymptomatic subjects who developed GN later or didn’t develop GN during a health check-up. Methylation analyses were performed on DNA extracted from these biopsy samples and also from GN tissue, and the mucosae in its vicinity taken from patients who developed GN later.
The data revealed that DNA methylation that highly accumulated in the gastric mucosa many years prior to GN formation was associated with higher GN risk and a shorter period for the onset of disease. Interestingly, the data also showed that methylation levels in the patients’ DNAs were linked to H. pylori infection and a lifestyle that involved tobacco and alcohol consumption.
While DNA methylation was determined to be an independent GN risk factor, drinking and smoking were found to amplify the pro-carcinogenic DNA methylation alterations caused by H. pylori. “The combination of unfavorable lifestyle factors and DNA methylation resulted in a much higher risk of GN development,” says Prof Tan. “Most importantly, when integrated into our analyses, this information accurately reflected the risk of GN and offers the possibility of tailoring management according to the risk of the patient,” adds Prof Yeoh.
The study’s findings could go a long way in securing a future with lower health care costs. Dr. Kaneda is quick to note that stratifying the GN risk across a population opens the door to implementing appropriate cancer prevention strategies at an early stage. Additionally, he is hopeful the findings emphasize how lifestyle choices like tobacco and alcohol consumption impact long-term health.
“We foresee a scenario where high-risk individuals get an early start on gastric cancer interventions. This could be achieved by developing an examination kit that identifies the diagnostic DNA methylation markers and provides a precise GN risk assessment,” conclude Drs. Usui and Kaneda.
More information:
Genki Usui et al, Integrated environmental, lifestyle, and epigenetic risk prediction of primary gastric neoplasia using the longitudinally monitored cohorts, eBioMedicine (2023). DOI: 10.1016/j.ebiom.2023.104844
Journal information:
EBioMedicine
Source: Read Full Article