Fewer patients sent to hospital rehabilitation facilities after colorectal operations early in the COVID pandemic
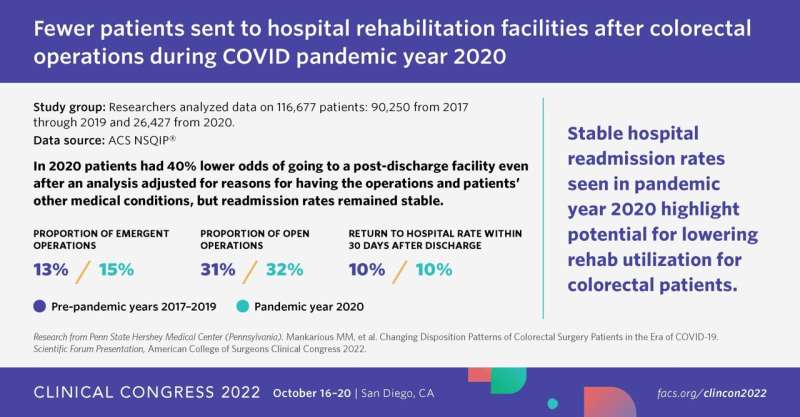
The first months of the COVID pandemic had a profound effect on hospital discharge practices and use patterns for patients with colorectal disease, according to findings presented at the Scientific Forum of the American College of Surgeons (ACS) Clinical Congress 2022. A study of more than 100,000 surgical patients who underwent procedures for colorectal cancer found that they had 40% lower odds of being discharged to post-hospital rehabilitation during the pandemic than before.
Despite this significantly lower rate, the hospital readmission rate did not change from pre-pandemic levels, said Marc Mankarious, MD, a surgical resident at Penn State Hershey Medical Center, Hershey, Pennsylvania.
“We found that discharge to a rehabilitation facility pre-pandemic was 10%, which agreed with previous literature, but once the pandemic hit, the discharge-to-rehabilitation rate dropped to about 7%,” Dr. Mankarious said. “We saw a drop of three percentage points, even though we were doing more emergent operations and more open operations, which are typical risk factors for requiring rehabilitation after surgery.”
The authors hypothesized that anecdotally, fear of going into confined spaces, staff and supply shortages, and disease outbreaks contributed to changes in discharge practices.
About the study
The retrospective cohort study used two databases from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP): the Participant Use File and Target Colectomy databases. Researchers analyzed data on 116,677 patients: 90,250 from 2017 through 2019, and 26,427 from 2020. For comparison, the first quarter was excluded from all years because the first COVID restrictions did not go into effect until March 2020. ACS NSQIP is the leading nationally validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care in hospitals. It was created by surgeons to help hospitals gauge the quality of their surgical programs and improve surgical outcomes by collecting robust, accurate, and precise clinical patient information.
Key findings
- In comparing the pre- and post-COVID-19 periods, the proportion of emergent cases and open operations—as opposed to minimally invasive procedures—increased in 2020, from 13 to 15% (p<0.001) and 31 to 32% (p<0.001), respectively.
- A multivariable analysis found that patients in 2020 had 40% lower odds of going to a post-discharge facility (odds ratio 0.62, p<0.001), even after the analysis adjusted for reasons for having the operations and other medical conditions the patients had.
- The rates of patients going back to the hospital within 30 days of discharge was 10% in both periods (p=0.4).
Surgeons’ observations
The stability in hospital readmission rates was telling because that may be “one of the factors that goes into deciding whether to offer a rehabilitation stay to a patient,” Dr. Mankarious said.
The study data did not include reasons why patients did or did not choose to go to post-discharge rehabilitation to recover; the authors hypothesized that factors included limited availability of beds and patient concerns about visitor restrictions and contracting COVID-19 Dr. Mankarious said. But the pandemic saw a 63-fold increase in telehealth use in 2020 over 2019.* “This situation may have made patients and physicians more comfortable with the patient going home and following up with each other electronically,” he said.
The data included some information on medical reasons for going to rehabilitation. “We did find that patients that went to rehabilitation in 2020 were more functionally dependent or functionally impaired than patients that went to rehabilitation in previous years, so those factors may also play a part in it.” Dr. Mankarious said.
The study grew out of what surgeons at Penn State Hershey were observing in the early days of the pandemic, said senior author Audrey Kulayat, MD, assistant professor of colorectal surgery. “We wondered if those observations had an impact on a bigger scale other than just at our institution,” she said. “But then we wanted to know, what’s the downside? Was there a downside? Are patients getting readmitted more frequently as a result of going back to their home or whatever institution versus going to a place with a higher level of nursing care? We didn’t find that they were readmitted more often.”
Potential change in discharge practice
The study findings raise questions about the potential overuse of posthospital rehabilitation for colorectal patients, Dr. Mankarious said. “Medicare spends about $60 billion per year on patients going to post-acute care facilities or rehab in general and any small reductions, even our 3% reduction, which was significant, could result in considerable cost savings for the healthcare system.
Source: Read Full Article
