Heart injury biomarker may help COVID-19 patients avoid hospitalization, new study shows
A study led by the University of St Andrews suggests that a frequently used medical test for heart injury could one day be used to help COVID-19 patients avoid hospitalization.
Cardiac troponins are proteins that form part of the heart’s contractile machinery and are released into the bloodstream when the heart is damaged. It can be measured in a blood test which is widely used in the assessment of heart attacks and other heart conditions.
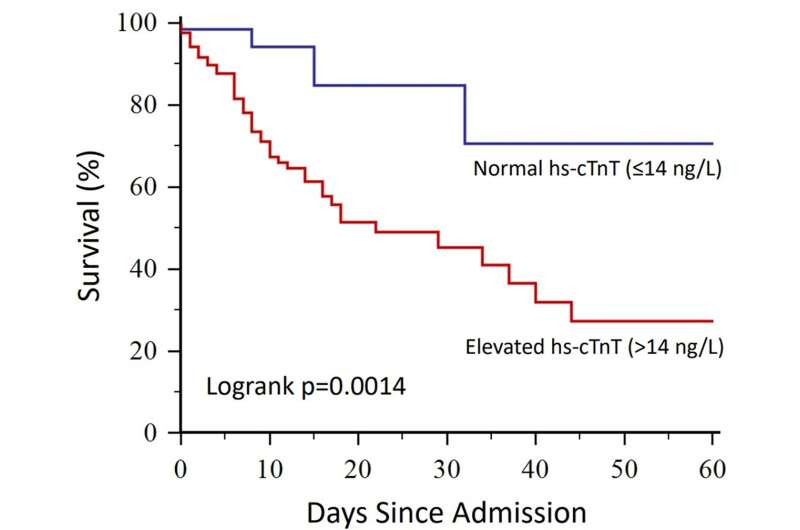
Existing studies since 2020 have shown that COVID-19 patients who have elevated troponin levels are more likely to die or suffer adverse clinical outcomes compared with those who have normal troponin levels.
However, despite this evidence, cardiac troponins are still not used in clinical practice to directly risk assess COVID-19 patients and this new paper, led by the University’s Dr. Alexander Liu and supervised by Dr. Robert Hammond, Professor Peter Donnelly and Professor Anthony Coates, investigates the diagnostic properties of cardiac troponin and its potential to be used in mainstream clinical practice.
Dr. Liu, from the School of Medicine, said, “COVID-19 is undoubtedly one of the worst pandemics of our generation. Identifying patients at a greater or lesser risk for mortality—what clinical staff call risk-stratifying patients—is important, as it may help us decide which patients need more medical attention and which patients can be discharged safely.
“Looking for heart injury is important because COVID-19 appears to have an ability to affect people’s hearts, and not just their lungs, and existing literature showed that patients with heart injury do less well in terms of prognosis than those without.
“Despite a body of evidence and potential, cardiac troponin is still not being used in clinical practice to directly risk-stratify patients with COVID-19. This study sought to ask why.”
The paper, published in the journal PLOS ONE, reports on a study of 191 patients with COVID-19, retrospectively looking at the ability of a subtype of cardiac troponin—high-sensitivity cardiac troponin T—to predict which patients suffered mortality, and which patients did not.
It found that having an elevated troponin test did not necessarily mean that the patient suffered mortality—it was inaccurate in predicting individual patient risk of death. This is most likely because, in real life, the patient population is diverse and there are factors other than heart damage which can cause elevated troponin tests. This observation may be the reason why clinicians are unable to use cardiac troponin alone to risk-stratify patients at present.
More importantly, the study also found that if a COVID-19 patient had normal cardiac troponin levels, the prognosis was very good. This is because normal troponin levels can potentially identify low-risk patients, since it may rule out complications and other illnesses that may put patients at a high risk.
Dr. Liu said, “The results indicated that rather than going along with the general message in the existing literature—which is that high troponin levels are linked to poor prognosis in COVID-19—we realized that as a diagnostic test, a high troponin level is unlikely able to accurately identify a patient at high risk of mortality. Instead, it may be better to exploit the ability of a normal troponin to rule out the risk of death in our patients.
“This study may be one small step towards clinical translation but potentially a giant leap for identifying the direction in which we need to go with COVID-19 risk-stratification. It now sets the stage for a future prospective validation of the rule-out powers of normal troponins. This could further propel the test into the COVID-19 clinical arena. The ultimate vision is to open up the possibility of using cardiac troponins to help doctors send patients home safely, to reduce their risk of hospital exposure, potentially saving lives and millions for healthcare systems.”
Dr. Liu added, “This project is not just a research piece but also a product of human resilience, forged on a shared desire to make things better for our patients while bracing the challenges of the pandemic. This study benefited from the input of junior doctors, senior scientists, and clinicians across various disciplines and sites. It is a privilege to do research with them.”
More information:
Normal High-Sensitivity Cardiac Troponin For Ruling out inpatient mortality in Acute COVID-19, PLoS ONE (2023). DOI: 10.1371/journal.pone.0284523
Journal information:
PLoS ONE
Source: Read Full Article