How a bereaved mom is helping researchers improve palliative care
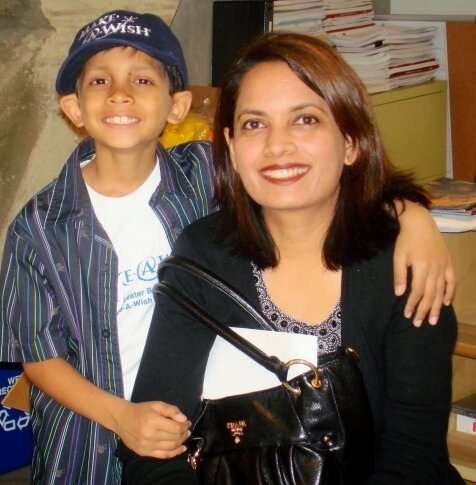
Jamila Hassan’s son Omar was two when he was diagnosed with acute lymphoblastic leukemia. He underwent chemotherapy, remission, a relapse, more chemo and a bone marrow transplant before dying shortly before his 10th birthday in 2012.
Hassan drew on the support of parents she met in the Bass Center for Childhood Cancer and Blood Diseases at Stanford Medicine Children’s Health, people who knew from experience about caring for—and losing—a child with cancer. Their understanding motivated her to pay it forward to families in similar situations: She recently joined a team of scientists preparing a paper on ethical conduct of research in end-of-life care, as a way of sharing what she had learned from Omar’s long journey as a childhood cancer patient.
Hassan’s contributions to the paper include comments about the value of families’ frontline knowledge of terminal illness care. She says, in part, “I think this kind of study would be an opportunity to improve small things parents remember about these important discussions or stressful times, like how a doctor or nurse talks to you slowly and calmly or helps you feel supported.”
Including families
Hassan’s work with a team of experts from across the country, which began at the invitation of Stanford Medicine nurse-scientist Kimberly Pyke-Grimm, RN, Ph.D., is an example of unusual new directions that experts are taking to involve bereaved families in research about medical decisions made near the end of their children’s lives.
The paper by Hassan; Pyke-Grimm, clinical assistant professor of pediatrics; and their collaborators, which was recently published in Pediatrics, addresses how best to study end-of-life decisions. To their knowledge, they are among the first to add to their team of scientists and bioethicists a parent who lost a child to cancer.
“I think there’s always room to improve our process for palliative care, including end-of-life care,” said Pyke-Grimm, who studies treatment decision making at Stanford Medicine Children’s Health.
For instance, families might appreciate earlier integration of palliative caregivers into their child’s team, specific social supports or a different way of sharing difficult medical news, she said. Research into families’ opinions of care for a terminal illness has been rare—partly a result of researchers’ concerns about whether such studies put too much strain on people who are under stress or grieving. But a desire to learn from families’ experiences means the work is gaining traction.
Bereaved parents have an understanding of end-of-life decisions that can’t be duplicated by any amount of academic expertise, which makes them invaluable not just as participants in research but also as full scientific collaborators, according to Pyke-Grimm.
“It makes good sense to have them guide us, to benefit from their wisdom and experience,” she said.
Benefiting from knowledge
The new paper proposes a design for a study in which researchers interview families about their experiences with end-of-life decision making. These families would be asked about their perceptions of a conversation with a caregiver about the end of life, including what caregivers said or did that helped the family make difficult decisions about the child’s care.
The interviews could be centered on any end-of-life decision. Families may be involved in deciding, for instance, when to discontinue chemotherapy for a child whose cancer is not responding to treatment, when and how to initiate palliative care, how to approach pain management at the end of life, or how medical care can support goals the patient hopes to reach in the remainder of his or her life.
The paper includes expert analysis of the ethical strengths and weaknesses of such a study.
During Omar’s seven years in and out of the hospital, the Hassan family, of San Jose, California, formed strong bonds with Omar’s caregivers.
“I had the most wonderful team to work with, amazing doctors and nurses. They did whatever they could to save him,” Jamila Hassan said. The team also did what they could to make the hospital more hospitable, following Omar’s suggestions such as serving fun foods (Oreos and pizza) and supporting his efforts, with his mom, to found a charitable organization, Omar’s Dream Foundation, which provides iPads to help children participate in school while they are hospitalized.
When Omar was very sick, Hassan was grateful for the times she received emotional support from caregivers on the team who had come to know her well. She especially appreciated the efforts that Omar’s caregivers made to connect her to another mom who had lost a child to cancer, someone who could provide a knowledgeable and sympathetic ear.
Even with all the love and support from Omar’s team, there were moments when Hassan wondered if her family’s caregivers truly understood what it was like to have a terminally ill child.
“They say things like, ‘You will be fine,’ and when you are hearing it as a parent, you’re thinking, ‘This person is saying it because it’s her job, but she hasn’t been through it herself,'” Hassan said.
Flexibility helps
In the paper, Hassan described how researchers could adapt studies to take families’ needs into account. Rather than following a rigid timeline for when families could join a study, for example, Hassan advocated for flexibility, pointing out that researchers should be sensitive to the mix of stressors families with dying children face.
“Parents could be worried about work, finances or their other children, or just having a hard day,” she wrote. “Also, they may not be eating or sleeping well (child or parent), or do not want to leave their child. An individualized approach would be important.”
Building on existing relationships between the child’s caregivers and the families would also be helpful, Hassan said, noting that as a parent, she would have been more likely to participate in research if she learned about it from her son’s doctor instead of a scientist she had never met. She also suggested having parents who had already participated in research available to guide new participants.
Pyke-Grimm hopes that recommendations such as Hassan’s will strengthen the research field and ultimately help all caregivers approach end-of-life care as sensitively as possible.
Source: Read Full Article
