How differences in diagnoses of mental disorders might affect clinical research outcomes for antipsychotics
Most physical disorders such as heart disease or muscular dystrophy have well-defined boundaries. Clinicians from across the globe regularly revise disease definitions to be on the same page as far as the diagnosis of these disease goes. This practice improves the corresponding clinical outcomes and helps maintain uniformity and common communication.
However, this is not always possible. For instance, in the case of many psychiatric disorders, it is slightly challenging to draw lines and set hard boundaries with respect to clinical features of a particular illness. Owing to this limitation, the prescribed psychiatric therapies tend to vary to a certain extent, depending on the clinician’s perspective.
Recently published research from Japan now aims to close this gap by identifying the source of this variance, and how to reduce its impact on patients with mental illnesses. This paper was published in Psychiatry and Clinical Neurosciences.
Says lead author Masashi Ikeda, a Professor at the Department of Psychiatry, Fujita Health University School of Medicine, “Diagnosis of psychiatric disorders is based on symptoms identified by diagnostic criteria, such as those outlined by the Diagnostic and Statistical Manual of Mental Disorders. However, this diagnosis is not made based on objective test data. In fact, the diagnosis may differ depending on the psychiatrist’s nuances and interpretation of the patient’s symptoms.”
Is there, however, a way to make these diagnoses more objective?
Common links between psychiatric disorders
Prior work undertaken by the Japanese research team has shown that subtypes of bipolar disorder share certain features to a varying extent with two other psychiatric disorders: schizophrenia and depression. An analysis of Japanese and Caucasian patient databases indeed show surprising trends. Whereas the Caucasian data show that bipolar I disorder has features that are more in common with schizophrenia, the Japanese data show that it tends to have features that are more in common with depression.
On the other hand, for bipolar II disorder, both Caucasian and Japanese data show a similar degree of commonality with schizophrenia and depression. Moreover, the study clearly establishes a genetic correlation between subtypes of bipolar disorder and schizophrenia/major depressive disorder in East Asian and European populations.
The study suggests that differences between Japanese psychiatrists and Western psychiatrists in their diagnostic tendencies, or in the tendencies of patients to whom the psychiatrists request to participate in research, contribute to the observed clinical discrepancies.
For instance, Japanese psychiatrists, heavily influenced by classic German psychiatry, tend to believe that bipolar disorder is a mood problem. They also may not diagnose bipolar disorder in patients with delusions and certain other characteristics with careful attention. These specific differences in opinions mean that Japanese and Western psychiatrists may hold two differing opinions about the diagnosis of the same patient, based on their personal experience and perceptions.
Co-author Takeo Saito, a senior lecturer at the Department of Psychiatry, Fujita Health University School of Medicine, adds, “If this trend is also occurring in clinical trials, then it may affect the evaluation of drug responsiveness, especially second-generation antipsychotics. Therefore, caution may be required while analyzing the data.”
How is this so?
Clinical trials recruit patients with specific disorders, to see if a drug is beneficial for that particular disorder. Understandably, if the criteria for diagnosis of a mental illness is different across the globe, then the recruitment of patients in clinical trials will differ as well—the proportions of patients with a particular illness will vary among clinical trials in different countries, thereby affecting the results of the trial.
This can be remedied with new directions for clinical interventions
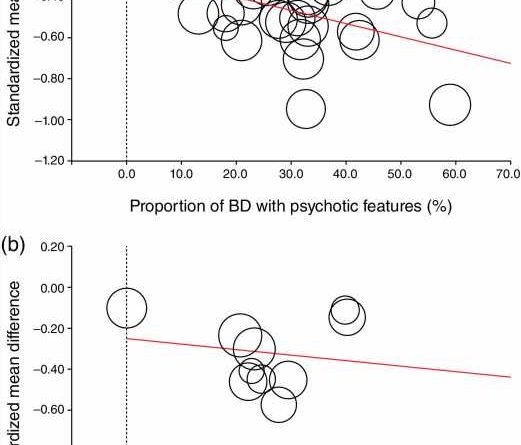
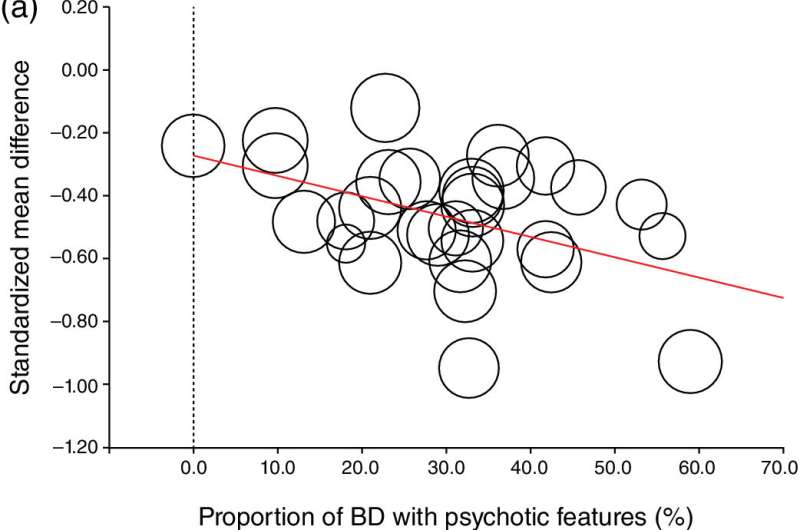
To test whether their hypotheses was correct or not, the researchers examined whether response rates to pharmacotherapy during acute mania in bipolar disorder differed based on the extent to which psychotic features were represented in the analyzed samples. In other words, they tried to determine the therapeutic efficacy of antipsychotics in patients with acute mania and bipolar disorder, who exhibited clear or no psychotic features.
To this end, the team performed meta-regression analyses of 28 double-blind randomized trials and compared the effects of classical mood stabilizers such as lithium and antipsychotics. The results were significantly startling: whereas classical mood stabilizers did not correlate with treatment response, antipsychotics showed relatively higher treatment response rates when the proportion of patients with psychotic features was also relatively higher. In other words, antipsychotics, but not mood stabilizers, were effective in treating patients with bipolar disorder who also exhibited psychotic features.
As a result, the treatment effect of antipsychotic drugs under consideration got “underestimated” when patients with bipolar disorder seeking treatment hardly exhibited any psychotic features.
Co-author Taro Kishi, also an associate professor at the Department of Psychiatry, Fujita Health University School of Medicine, says, “It is unclear whether the inclusion of patients with or without psychotic features in clinical trials reflects a sampling problem or a diagnostic problem. However, in clinical trials for bipolar disorder, the proportion of patients with and without psychotic features should always be included in the clinical background and considered during subsequent analyses, especially since it could be highly relevant to the evaluation of treatment efficacy of antipsychotic medications.”
Source: Read Full Article