Incidents of serious parasitic disease on the rise in Alberta, Canada
A rare parasitic infection imported from Europe continues to take root in Alberta, Canada. The province is now the North American hotspot for human alveolar echinococcosis (AE), which takes the form of a growth in the liver, causing serious and potentially deadly health complications.
A recently published review of known AE cases in Alberta found 17 instances of human AE diagnosed in the province between 2013 and 2020. Before the recent surge, only two cases of human AE had been previously confirmed in North America—one in Manitoba in 1928 and another in the U.S. state of Minnesota in 1977.
“This parasite has now become very widely established in the wild in the Prairies. It’s been found in Saskatchewan and in B.C., but Alberta has had most of the cases of human disease,” said University of Alberta infectious diseases expert Stan Houston, who helped lead the study.
“We have been having on average more cases every year. There’s been a lull since COVID-19, but I’m suspicious it reflects a slowdown in testing during the pandemic and that we may soon see a surge again.”
According to Houston, the strain of AE found in the Alberta cases has been identified by scientists at the Faculty of Veterinary Medicine in Calgary as having originally come from Europe, likely in dogs brought to the area.
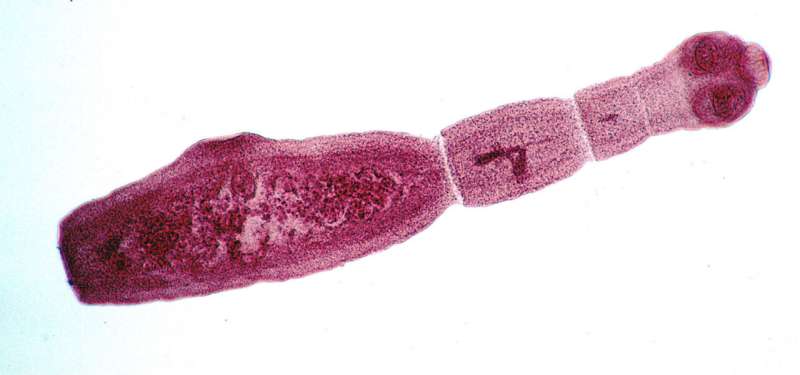
The parasite takes the form of a tiny tapeworm in canines—typically foxes and coyotes, but potentially pet dogs—and is considered to be relatively harmless to them. When a rodent ingests parasite eggs from canine feces, it gets a different form of the disease and develops a tumour, or parasitic growth, in the liver, which kills it. When the rodent is eaten by a canine, the parasite takes the tapeworm form again.
“We humans are taking the place of the rodent in the life cycle when we accidentally consume microscopic parasite eggs—maybe in strawberries or lettuce from a garden where a coyote passed through, or possibly a dog if it is carrying the parasite,” said Houston, also noting that a human could become infected by petting a dog that has microscopic traces of canine feces in its hair and then touching food or their mouth, accidentally ingesting the parasite’s eggs.
The European strain of AE has been notably successful in Alberta, quickly spreading in the wild. Increased human contact with coyotes as they have become urbanized, along with the increasing numbers of people with diseases or therapies that weaken the immune system, are likely to contribute to the number of humans developing the disease.
“In coyotes in Calgary and in Edmonton, more than half have been found to be carrying this parasite. So the new strain seems to not only be more virulent when it affects humans, but it seems to be super-effective in wild hosts,” said Houston.
“Diseases from animals have always been important to keep an eye on,” he added. “The COVID-19 pandemic has again elevated awareness of the number and importance of human diseases that are transmitted from animals.”
Of the 17 cases found in Alberta, 11 patients lived in rural areas, 14 of them owned dogs and six were immunocompromised individuals—of special interest as the disease progresses faster in patients whose immune systems have been suppressed.
The symptoms of AE can be difficult to spot. The infection typically has an incubation period of several years before a patient begins showing signs of illness. Almost half of the cases in Alberta were found accidentally when the patient was getting tested for a different illness. It’s often found after an ultrasound shows abnormalities in the liver, followed by an investigative biopsy. When symptoms occur, they can include unspecified pain, jaundice, weakness and weight loss—many of the same conditions that could be expected from a cancerous tumour in the liver.
“In the majority of cases that was the people’s first thought when they saw the imaging, that it was cancer,” said Houston. “The symptoms would be indistinguishable from many other diseases in the liver, hence the need for a biopsy diagnosis.”
If found early enough, treatment can involve surgery to remove the mass from the liver. Because the parasite is initially symptomless, it is often able to slowly grow and by the time it is found, about two-thirds of patients will be inoperable. In those cases, lifelong antiparasitic drugs are the only option. The drugs won’t kill the parasite but will prevent it from growing further. If left untreated, the parasite could kill its human host within 10 to 15 years.
Currently the most useful drug for controlling AE is not licensed in Canada (although widely available in most of the rest of the world) and only available through a special physician application process to both the government and manufacturer.
Avoiding the parasite comes down to good hygiene practices and taking simple precautions. Houston said it’s a good idea to wash your hands after handling your dog, especially if you suspect it’s eaten a rodent or spent time in a dog park or area where coyotes frequent. Also recommended is thoroughly washing produce that comes from the ground or close to the ground, such as lettuce or mushrooms.
The researchers are now working on a new study examining samples of liver biopsies from patients in Alberta where cancer wasn’t found, to look for possible previously unrecognized cases of AE.
“That would give us a better picture of what’s going on, but more importantly, would give us a chance to give those patients appropriate therapy,” said Houston.
“We should be paying attention, but it’s still a very rare disease,” he added. “People should keep that in perspective, adopt health behaviours and not obsess about this.”
Source: Read Full Article
