Its not just SARS-CoV-2: Most respiratory viruses spread by aerosols
SARS-CoV-2, the virus behind today’s global coronavirus pandemic, spreads primarily by inhalation of virus-laden aerosols at both short and long ranges —and a comprehensive new assessment of respiratory viruses finds that many others probably do as well. SARS-CoV, MERS-CoV, influenza, measles, and the rhinoviruses that cause the common cold can all spread via aerosols that can build up in indoor air and linger for hours, an international, interdisciplinary team of researchers has reported in a review published in Science Aug. 27.
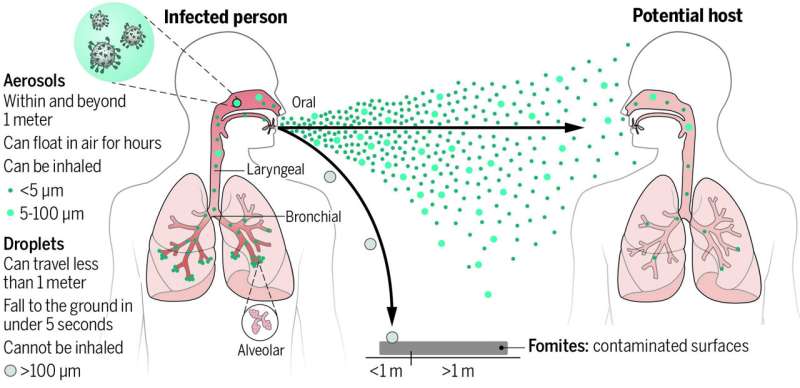
Over the last century and at the beginning of this pandemic, it was widely believed that respiratory viruses, including SARS-CoV-2, mainly spread through droplets produced in coughs and sneezes of infected individuals or through touching contaminated surfaces. However, droplet and fomite transmission of SARS-CoV-2 fails to account for the numerous superspreading events observed during the COVID-19 pandemic, or the much higher transmission that occurs indoors versus. outdoors. Motivated by a desire to understand the factors leading to the COVID-19 pandemic, the researchers from Taiwan, the United States, and Israel sought to identify as clearly as possible how the coronavirus and other respiratory viruses spread. For example, the team reviewed numerous studies of superspreading events observed during the COVID pandemic, and found the studies consistently showed that airborne transmission is the most likely transmission route, not surface contacts or contact with large droplets. One common factor at these superspreading events was the shared air people inhaled in the same room. Many were linked to crowded locations, exposure durations of one hour or more, poor ventilation, vocalization, and lack of properly worn masks. The researchers also reviewed evidence collected from many other types of studies—air sampling, polymerase chain reaction (PCR)-based and/or cell culture studies, epidemiological analysis, laboratory and clinical studies, and modeling work—and concluded that airborne transmission is a major, or even dominant transmission pathway for most respiratory diseases, not just COVID-19.
“Transmission through inhalation of virus-laden aerosols has been long underappreciated. It is time to revise the conventional paradigms by implementing aerosol precautions to protect the public against this transmission route”, said Chia C. Wang, director of the Aerosol Science Research Center and an aerosol physical chemist at National Sun Yat-sen University, Taiwan, who led the review.
Prevailing paradigms about respiratory disease transmission date back as much as a century, the team noted. Airborne transmission was paternalistically dismissed in the early 1900s by prominent public health figure Charles Chapin due to a concern that mentioning transmission by air would scare people into inaction and displace hygiene practices. An unsupported assumption that erroneously equated infections at close range with droplet transmission has shaped the current paradigm for controlling respiratory virus transmission. However, “this assumption neglects the fact that aerosol transmission also occurs at short distances, because the concentration of exhaled aerosols is higher when one is closer to the infected person emitting them,” said Kim Prather, director of the National Science Foundation Center for Aerosol Impacts on Chemistry of the Environment at UC San Diego’s Scripps Institution of Oceanography at UC San Diego and an aerosol chemist who co-led the review.
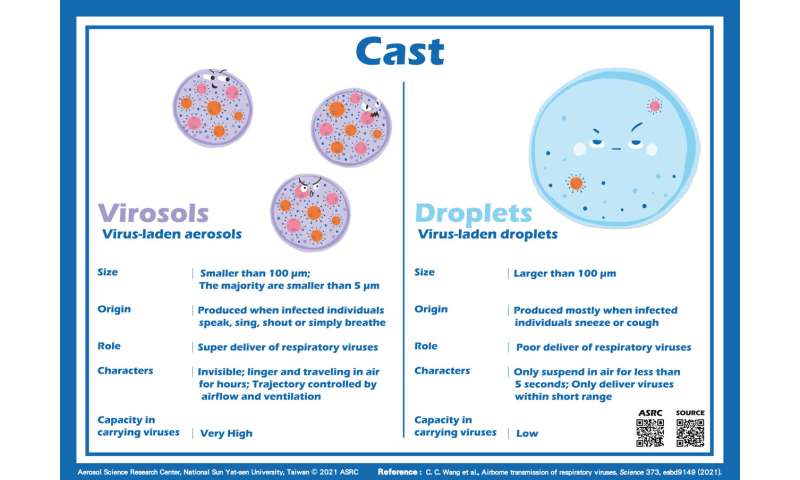
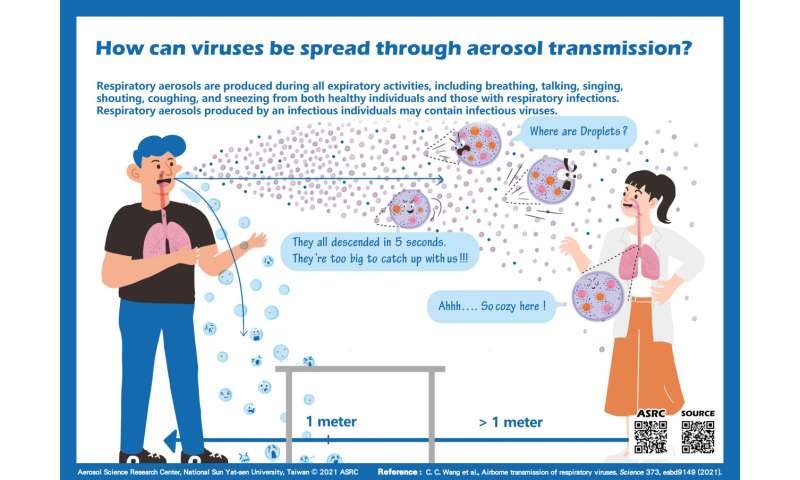
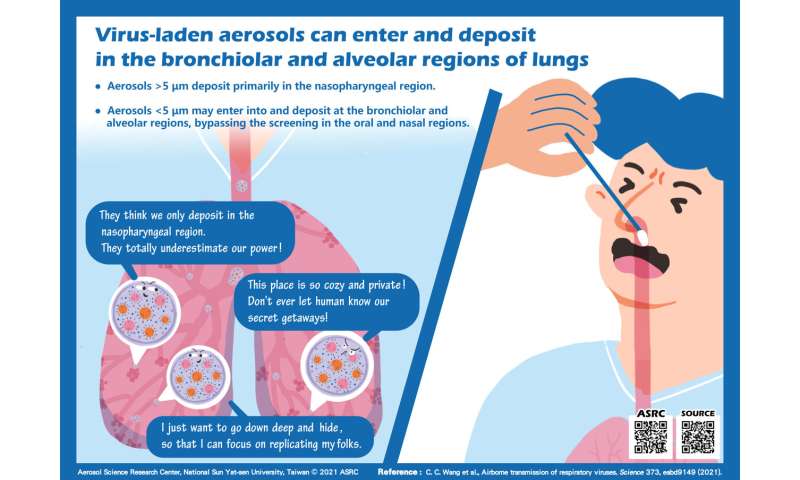
Respiratory aerosols are formed by expiratory activities, such as breathing, talking, singing, shouting, coughing, and sneezing. Before COVID-19, the traditional size cut-off between aerosols which float like smoke and droplets which drop had been set at 5 µm, however, 100 µm is a more appropriate size distinction. This updated size better represents the largest particles that can remain suspended in still air for more than 5 seconds (from a height of 1.5 meters), travel beyond one meter from the infected person, and be inhaled. “The physical size predominantly determines how long they can stay suspended in the air, how far they can reach, whether they are inhalable, and how deep they can enter into the respiratory tract if inhaled. “The majority of aerosols produced by respiratory activities are smaller than 5 µm, which allows them to travel deep into the bronchiolar and alveolar regions and deposit there. Studies find that viruses are more enriched in aerosols smaller than 5 µm”, said Josué Sznitman, a pulmonary physiologist of Technion, Israel.
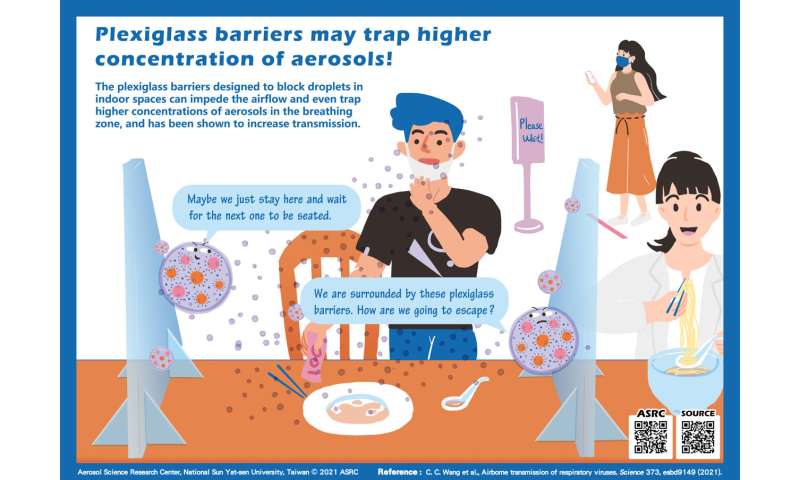
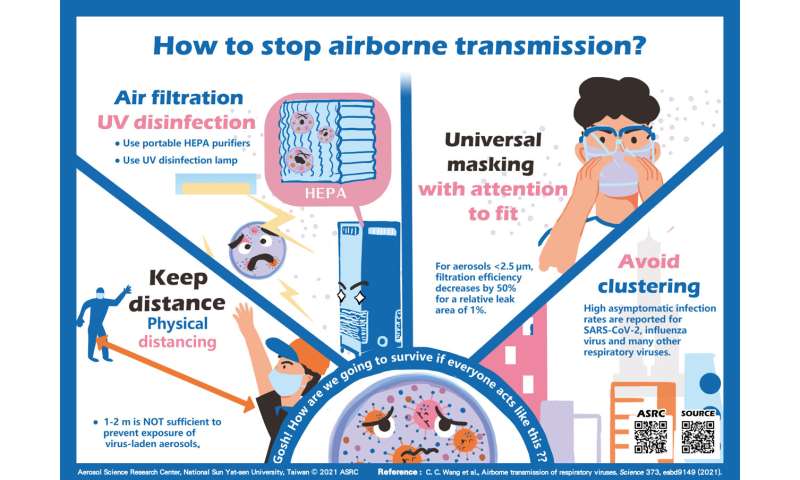
Another distinct behavior of aerosols that should be taken into serious consideration is their capacity to be influenced by airflow and ventilation. Ensuring sufficient ventilation rates, filtration, and avoiding recirculation help reduce airborne transmission of infectious virus-laden aerosols. “Monitoring CO2 with portable meters helps verify that ventilation is sufficient, and implementing portable HEPA (high efficiency particulate air) purifiers and upper room UV disinfection systems also help reduce the concentrations of virus-laden aerosols”, added Jose-Luis Jimenez, an atmospheric aerosol chemist of the University of Colorado Boulder. On the other hand, the plexiglass barriers commonly used to block droplet spray from coughs and sneezes in indoor spaces may “impede proper ventilation and create higher exposures for some people,” said Linsey Marr of Virginia Tech, who has studied airborne transmission of pathogens for years. “They are not recommended except for brief, face-to-face transactions, but even then, masks are better because they help remove aerosols, while barriers just divert them.”
With the surge in infections caused by the Delta variant and the increasing occurrence of “COVID-19 breakthrough cases” (infections among people who have been fully vaccinated), many governments and national disease control agencies have resumed universal masking in public. Universal masking is an effective and economic way to block virus-laden aerosols, reported in the review. However, “we need to consider multiple barriers to transmission such as vaccination, masking, and ventilation. One single strategy is unlikely to be strong enough to eliminate transmission of emerging SARS-CoV-2 variants. “, added Seema S. Lakdawala, a virologist of the University of Pittsburgh.
As the evidence for airborne transmission of SARS-CoV-2 has increased over time and become particularly strong, agencies have taken notice. In April and May 2021, the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) acknowledged inhalation of virus-laden aerosols as a main route in spreading COVID-19 at both short and long ranges. This means that to mitigate transmission and end this pandemic, decision makers should consider implementing aerosol precautionary measures, including universal masking with attention to mask fit, improving ventilation rates in indoor spaces, avoiding recirculation of contaminated indoor air, installation of air filtration such as HEPA purifiers that can effectively remove airborne particles, and using UV disinfection lamps. “What are traditionally called droplet precautions are not replaced wholesale, but instead are modified, expanded and deployed in a more effective manner in accordance with actual transmission mechanisms”, noted by Zeynep Tufekci, a sociologist at the University of Columbia who studies societal challenges in COVID-19 pandemic. Having the correct mental model of transmission of this disease and other respiratory diseases will also allow ordinary people to make better decisions in everyday situations and administrators and officials to create better guidelines and working and socializing environments even after the pandemic, she added.
Source: Read Full Article
