Keys to making immunotherapy work against pancreatic cancer found in tumor microenvironment
A new study that analyzed the tumor microenvironment of pancreatic cancer revealed the cause of tumor cell resistance to immunotherapy and resulted in new treatment strategies.
This study, led by researchers at the Johns Hopkins Kimmel Cancer Center, is the latest from an ongoing platform trial formed in 2015 to study immunotherapy treatments before surgery (neoadjuvant) and after surgery (adjuvant) in patients with pancreatic cancer.
The platform trial enables researchers to use data generated by the trial to advance the development of immunotherapies for pancreatic cancer within the same trial, says Lei Zheng, M.D., Ph.D., co-director of the Pancreatic Cancer Precision Medicine Center of Excellence Program and professor of oncology at the Johns Hopkins University School of Medicine.
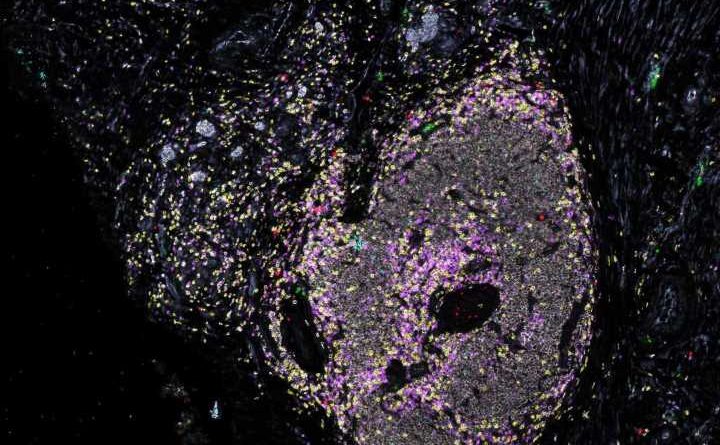
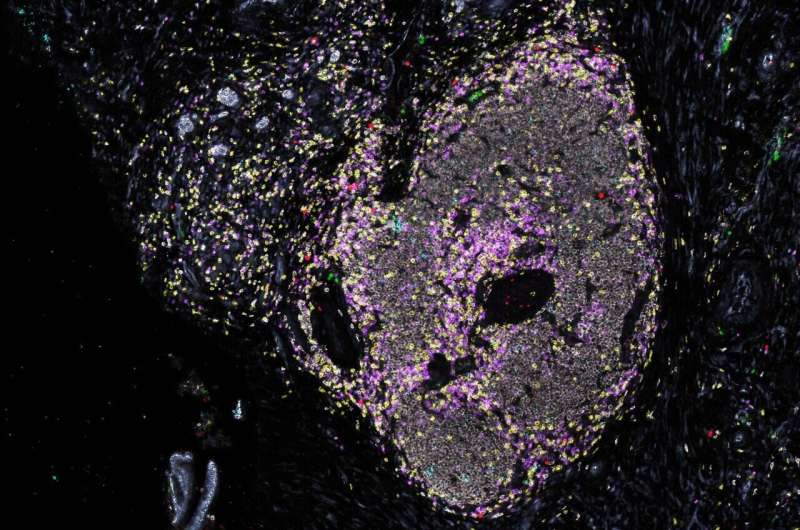
In the study, a multidisciplinary team co-led by Zheng, Elizabeth Jaffee, M.D., professor of oncology and deputy director of the Johns Hopkins Kimmel Cancer Center, and Elana Fertig, Ph.D., associate professor of oncology and director of oncology quantitative sciences, used banked biospecimens and studied the tissue, cellular and molecular structure of the tumor microenvironment by employing multiomic strategies, meaning they explored the genetic alterations (DNA), transcriptomes (RNA) and proteins expressed.
Findings from the most recent study were published in Cancer Cell.
Pancreatic cancers tend to suppress the body’s immune response and prevent immune effector cells, such as T cells, from killing the tumor cells, which the researchers call a cold microenvironment. In this platform trial, researchers gained key insights into the microenvironment—the cells in and around pancreatic tumors that inhibit the immune response.
Two forms of treatment known to stimulate the body’s T cells to attack cancer cells, alone or in combination, were studied, including anti-PD-1 immunotherapy, which blocks an immune checkpoint that cancer cells use to turn off the immune response to cancer, unharnessing an immune response to the cancer. The other immunotherapy studied was GVAX, a therapeutic vaccine that can stimulate the patient’s immune system to attack the cancer.
The study found two major “defects” in the pancreatic cancer’s tumor microenvironments. One is that T cells are exhausted and still not sufficiently active, and the second is that myeloid cells that infiltrate the tumor’s microenvironment prevent T cells from activating against pancreatic cancer cells, even after treatment with GVAX and anti-PD-1 immunotherapy.
Zheng says a major component of the myeloid cell, called neutrophils—created by immune cells to fight infection—is hijacked by pancreatic cancer cells to suppress T cell activation.
As a result of these findings, the researchers began testing two new treatment strategies: anti-CD137 agonist antibody treatment in combination with anti-PD-1 immunotherapy to activate T cells, and anti-IL-8 neutrophil-blocking antibody treatment in combination with anti-PD-1 immunotherapy to prevent the inactivation of T cells.
“We have seen promising activity we believe will improve the patient’s disease-free survival after the surgery,” says Zheng.
More information:
Keyu Li et al, Multi-omic analyses of changes in the tumor microenvironment of pancreatic adenocarcinoma following neoadjuvant treatment with anti-PD-1 therapy, Cancer Cell (2022). DOI: 10.1016/j.ccell.2022.10.001
Journal information:
Cancer Cell
Source: Read Full Article