Long-range airborne transmission of SARS-CoV-2
Infectious droplets generated by coughing, sneezing, or just ordinary speech and breathing have generally been categorized based on size between “droplets” and “aerosols,” with aerosols representing the smallest particles that can stay airborne, usually evaporating before reaching the ground.
The size at which a droplet becomes an aerosol is not clear-cut, with particle diameters ranging from 2 to 100 µm being given as the cut-off point across a range of published papers.
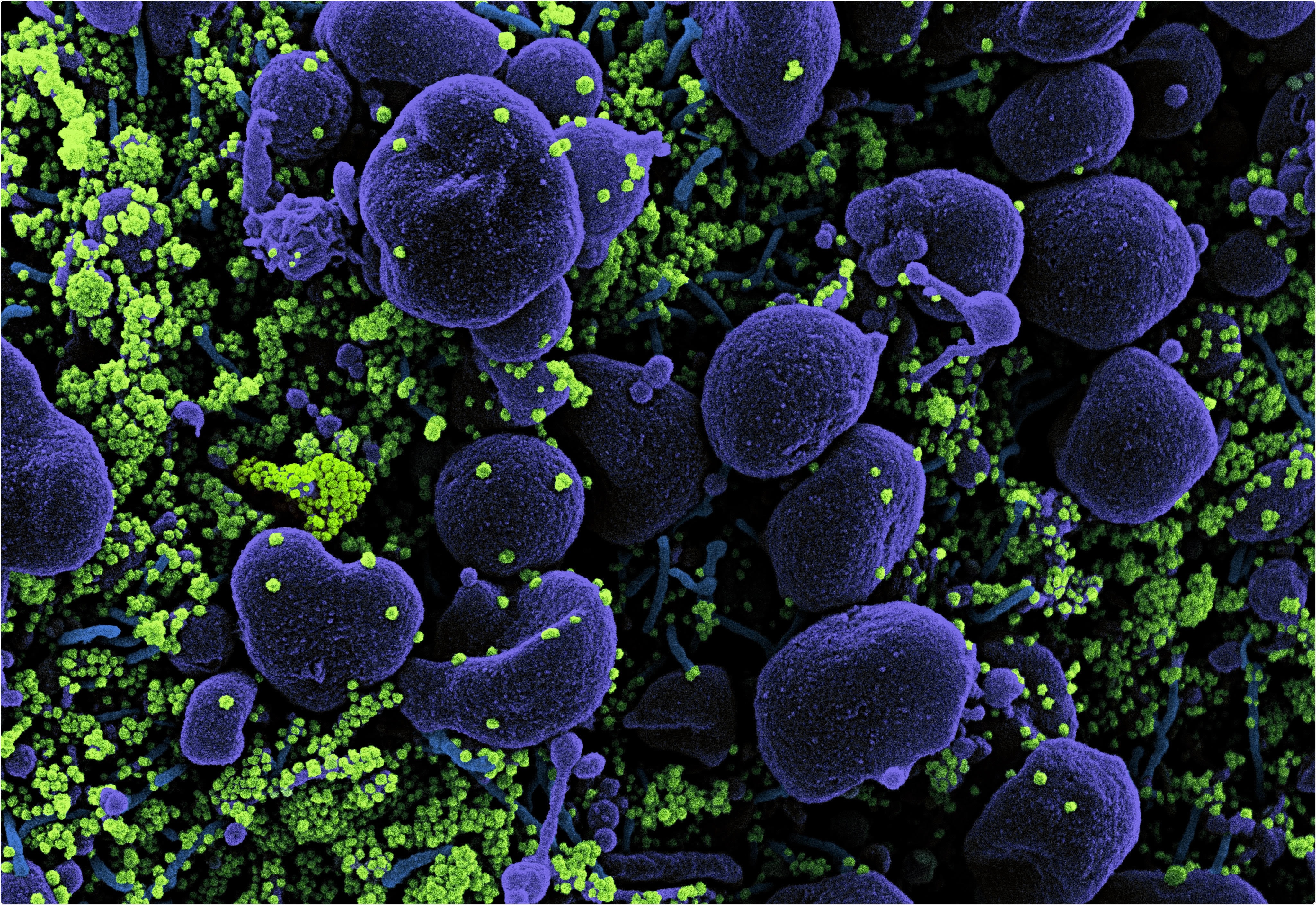
It is recognized that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be transmitted by aerosol, and recent work suggests that particles of the larger diameter viably produce SARS-CoV-2 aerosols massively increasing the quantity of pathogenic material delivered if inhaled.
In an early release copy of a short commentary paper recently published in the Canadian Medical Association Journal by Addleman et al. (June 8th, 2021), the impact of, and possible solutions to, the short- and long-range airborne transmission of SARS-CoV-2 are explored.
SARS-CoV-2 methods of transmission
SARS-CoV-2 is spread by exposure to infectious respiratory fluids, be that by touch, coming into contact with droplets or sprays, or by aerosol inhalation. Aerosol transmission is more likely at close range, dissipating over space and with time.
While still infectious for some time while airborne, the probability of becoming infected by an aerosol increases drastically with concentration. Thus, governments have generally recommended meeting others outdoors and other non-pharmaceutical interventions, where wind will help keep the surrounding concentration of SARS-CoV-2 aerosol consistently lower.
Longer range transmission of SARS-CoV-2 is possible, however, and has been demonstrated by contact tracing and genomic sequencing of the virus, where individuals with no physical contact have contracted a distinct variant.
The authors also argue that the large number of nosocomial infections, those occurring in a hospital setting, are evidence of airborne transmission, as, despite high levels of protocol adherence and droplet PPE, many medical staff were infected.
Animal studies have also demonstrated that the virus can be passed through an air duct to infect the test subjects, and viable SARS-CoV-2 has actually been sampled from the air in a hospital room and a car driven by a mildly symptomatic patient for 15 minutes.
Mitigating airborne transmission
From a public understanding point of view, the authors encourage the use of the term airborne, as it accurately reflects the ability of SARS-CoV-2 to persist in and travel through the air before infecting an individual.
They highlight the importance of ventilation, meeting outdoors, or wearing masks indoors, even when distanced. They recommend that advice disseminated to businesses and schools should strongly emphasize ventilation as the significant mitigating factor against long-range airborne transmission, far more so than measures intended to reduce transmission by droplets such as regular wiping or plexiglass sheeting, especially when these investments provide a false sense of security.
Fomite transmission, transmission from a surface, is a relatively low risk for SARS-CoV-2 once dry, depending enormously on the surface in question. At the same time, the group also point out that plexiglass barriers impede airflow and could further concentrate an aerosol.
The group recommends that indoor air quality monitors should be installed in public places to ensure airflow is consistent by probing carbon dioxide levels, and further that medical practitioners should be supplied with PPE appropriate to an airborne pathogen, not being concerned only with droplet or contact transmission. They state that this is particularly true in long-term care settings and nursing homes, where outbreaks have been particularly devastating.
Canadian medical staff reportedly only require the use of high-quality respirators such as N95 masks in aerosol-generating procedures, and while surgical masks provide some protection from aerosol inhalation studies have demonstrated staff wearing only surgical masks contract SARS-CoV-2 more frequently than those wearing N95 masks.
The CDC currently recommends N95 respirators, gloves, gowns, and glasses when dealing with COVID-19 patients, and the authors encourage the same standard for Canadian workers. They also note that close-proximity occupations tend to have been disproportionately affected by the pandemic for this reason and that businesses should consider such measures for their staff, potentially saving money in the long-term when accounting for paid sick leave, etc.
However, distancing measures while indoors do little to lessen the transmission of SARS-CoV-2 without additional PPE, and when in an enclosed space the concentration of aerosol in the room will eventually reach concentrations that make infection highly likely.
- Sarah Addleman, Victor Leung, Leyla Asadi, Abdu Sharkawy and Jennifer McDonald CMAJ June 08, 2021 cmaj.210830; DOI: https://doi.org/10.1503/cmaj.210830, https://www.cmaj.ca/content/early/2021/06/08/cmaj.210830
Posted in: Medical Research News | Disease/Infection News
Tags: Breathing, Coronavirus, Coronavirus Disease COVID-19, Coughing, Genomic, Genomic Sequencing, Hospital, Nursing, Pandemic, Pathogen, PPE, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sneezing, Speech, Syndrome, Virus

Written by
Michael Greenwood
Michael graduated from Manchester Metropolitan University with a B.Sc. in Chemistry in 2014, where he majored in organic, inorganic, physical and analytical chemistry. He is currently completing a Ph.D. on the design and production of gold nanoparticles able to act as multimodal anticancer agents, being both drug delivery platforms and radiation dose enhancers.
Source: Read Full Article
