Mapping C. difficile: Advanced ribotyping technology helps researchers keep track of deadly disease
Interview with Seth Walk, Principal Investigator and Associate Professor, Department of Microbiology and Cell Biology, Montana State University

Image Credit: Promega Corporation
Can you give us a brief introduction to your background and research interests?
I joined Montana State University in 2012, and I am now Associate Professor and Head of the Walk Lab at the university. We’re interested in the human gut microbiome, which is currently quite a popular field.
We study some basic research questions in the field of microbial ecology, such as which organisms live in the gut and how they interact with their host (us), as well as questions related to infectious diseases and antimicrobial-resistant pathogens that cause disease in the gut.
We collaborate with other groups, for example, with partners who investigate inflammatory bowel disease and are trying to establish the host-pathogen interaction.
We also have a range of projects exploring how pathogens circulate in hospitals, with the aim of developing tools to track outbreaks and monitor newly emerging clones that could be resistant to treatment.
One of the main pathogens that we are interested in is Clostridioides difficile. This Gram-positive bacterium is the most common cause of hospital-acquired (nosocomial) infection in the U.S. and can cause severe gastrointestinal disease with high morbidity and mortality rates.
The bacteria’s epidemiology is always changing, so we really need the tools to differentiate between different C. difficile strains.
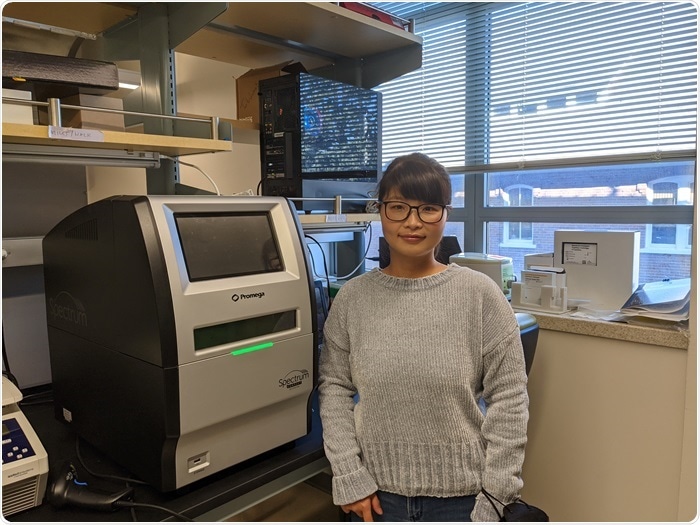
Image Credit: Promega Corporation
Can you explain what these ‘tools’ are and how they could be used?
We develop low-cost tools for characterizing isolates and are building databases to facilitate the work of others in the scientific community. We also use mouse models of C. difficile to understand how this pathogen is spread and what factors are important for preventing disease.
At the hospital level, there is a real need to ‘type’ the isolates, to measure their genetic and phenotypic diversity. We have developed a tool using a molecular technique known as ribotyping, which identifies and characterizes different strains of C. difficile based on genetic information around the ribosomal RNA (rRNA)-encoding genes.
This information tells us about their phylogenetic relationships; how closely related they are and whether new variants are popping up.
Ribotyping tools can be used in clinical diagnostics and infection control, to establish how different pathogenic strains are moving around a hospital and whether outbreaks are caused by recurrent or new strains.
Resistance surveillance is also a top priority for both the clinical and research communities, to assist with the development of new antibiotics. In the case of infection control, strain typing must be rapid, which is where our high-throughput fluorescent polymerase chain reaction (PCR) ribotyping tool comes in.
How does fluorescent PCR ribotyping work and why do you use this method over other techniques?
PCR ribotyping is a low-cost, gel-based genotyping assay for the identification of specific C. difficile lineages. It quantifies the differences in length between 16S rRNA and 23S rRNA encoding genes at approximately 11 rRNA-encoding operons around the C. difficile genome.
By using a fluorescently labeled PCR primer and sizing amplicons with Sanger-style (capillary-based) sequencing, fluorescent PCR ribotyping improves on the original ribotyping technique and our lab has developed a similar approach and applied it to C. difficile.
Sequence-based methods, such as multi-locus sequence typing (MLST) and genome sequencing, are expensive compared with gel- and now capillary-based methods. Common gel-based methods include pulsed-field gel electrophoresis (PFGE) and restriction endonuclease analysis (REA) typing, but their resulting data is not portable between laboratories.
The portability of data is particularly important for epidemiology studies so that links can be made between disease cases across the globe and patterns of emergence can be identified quickly. We carried out a multi-center study that demonstrated the portability and cost-efficiency of our standardized fluorescent PCR ribotyping protocol.1
Four different labs and three different sequencing centers achieved highly accurate and precise C. difficile ribotype identifications using our protocol and centralized database. What is really important for portability is that labs speak a ‘common language’. If we use the same naming conventions and the same platforms and databases, information can travel much more broadly.
What role does your database play in C. difficile ribotyping?
We have been building our database of C. difficile ribotypes for around a decade, and it currently contains 123 ribotypes and is freely available online. We have been running clinical samples from around the world with fluorescent PCR ribotyping on a capillary electrophoresis (CE) sequencer and we can quickly match identified strains with the references in the database.
We want other labs to be able to compare their ribotype identifications with our reference database and establish whether the pattern matches a previously named C. difficile ribotype, or a newly identified strain which can then be easily added to the database for future studies.
We recently developed a software package in R to rapidly analyze CE data, where users can input and parse raw data files and obtain a similarity metric between unknown queries and the reference database in one simple workflow.
In the early days, we were reliant on other companies keeping their proprietary databases and software up to date, whereas now, we can analyze and troubleshoot every raw data file received. The pipeline can even be adjusted to other CE-based databases – it is not limited to C. difficile.
How does the choice of sequencer impact your fluorescent PCR ribotyping pipeline?
Sanger sequencing by CE is a proven technology, and now instruments exist with a small enough footprint to fit in almost any lab – you don’t have to be affiliated with a large sequencing center or medical institution to run these experiments. Eliminating the hassle and cost of shipping samples and waiting for results is another benefit of bringing sequencing in-house.
Other larger sequencers are being discontinued because of the significant instrument overheads. The cost recovery equations aren’t working out for large core centers that are moving towards whole genome sequencing. Smaller instruments could become more appropriate in these settings.
We have recently started using Promega’s Spectrum Compact CE System and optimized our protocol on this instrument, which has allowed us to keep costs down and make our work available to the field much quicker than before.
Having the Spectrum Compact available is helping us to achieve our goal of making the C. difficile database a public service and to keep costs down for the field. Ultimately, we want our database to be compatible with other global databases.
What do you think the future holds for ribotyping and clinical epidemiology?
What this does is put another tool in the toolkit. I believe fluorescent PCR ribotyping could be really helpful for clinicians who are interested in knowing how specific strains of C. difficile and other pathogens are spreading throughout the hospital. I think this could be a real game-changer for infection control practices because the method is so rapid.
The other area where this technology could be of significant value is enabling clinicians to establish whether or not a case is recurrent. Once a patient starts to recur with C. difficile disease, they often end up recurring multiple times, and then it becomes a very different clinical scenario.
If they are picking up new strains, their microbiome is still susceptible to C. difficile infection, compared with whether there’s a strain that has come back from previous infections. Either they are becoming contaminated again from their own environment, which would require thorough decontamination, or the pathogen wasn’t killed during the first round of treatment, so an alternative therapeutic strategy might be needed.
In terms of what the future holds, I think once people see how this method works with C. difficile, they will most likely adapt it to the specific needs of their hospital or facility. Any method that is PCR-based will be very adaptable to other infections. It helps us keep our finger on the pulse of infectious disease epidemiology and hopefully keep on top of future outbreaks.
For more information about the Walk Lab and to download the software, please visit https://thewalklab.com/.
For more information about Promega’s Spectrum Compact, please visit www.promega.com/SpectrumCompact
References
- Martinson JNV, Broadaway S, Lohman E, et al. Evaluation of Portability and Cost of a Fluorescent PCR Ribotyping Protocol for Clostridium difficile Epidemiology. J Clin Microbiol, 2015; 53(4): 1192-1197.
About Promega Corporation
With a portfolio of more than 3,000 products covering the fields of genomics, protein analysis and expression, cellular analysis, drug discovery and genetic identity, Promega is a global leader in providing innovative solutions and technical support to life scientists in academic, industrial and government settings.
Promega products are used by life scientists who are asking fundamental questions about biological processes as well as by scientists who are applying scientific knowledge to diagnose and treat diseases, discover new therapeutics, and use genetics and DNA testing for human identification.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.
Source: Read Full Article
