Metabolic reprogramming of tumor-associated macrophages
Cancer is a complex disease and although billions of dollars have been spent on finding safe and effective therapeutics for it, there is still scope for significant development. Researchers have targeted a variety of biological entities and processes to treat cancer. One example is the metabolic processes that reprogram tumor-associated macrophages (TAMs), immune cells that play a crucial role in the development and progression of cancer.
Under normal circumstances, macrophages—white blood cells that engulf and kill microorganisms, eliminate dead cells, and stimulate the immune system—safeguard the body against disease. However, TAMs do something significantly odd: they participate in the formation of the tumor microenvironment (TME), thus harming the body. Depending on the environmental stimulus and metabolic processes, macrophages differentiate into two classes: anti-tumor M1-like and pro-tumor M2-like macrophages. The latter resemble TAMs. Whereas M1-like macrophages inhibit tumor growth, M2-like macrophages do the exact opposite and thus play a key role in the proliferation of cancer cell.
Researchers from China recently conducted a literature survey, which was published in the Chinese Medical Journal on 20 October 2022, to better understand how this happens. Says Prof. Yi Zhang, corresponding author of the article, and Professor and Director of the Biotherapy Center and Cancer Center at The First Affiliated Hospital of Zhengzhou University, “Peripheral blood-polarized and tissue-resident TAMs constitute a tremendous segment of infiltrating myeloid cells in the TME of most malignant solid tumors. Importantly, TAMs display proangiogenic properties. In this review, we elucidate the metabolic reprogramming of TAMs and explore how they sustain immunosuppression to provide a perspective for potential metabolic therapies.”
Tumor cell metabolism—defined as the set of biochemical processes that occur to ensure the survival of organisms—plays a key role in cancer cell proliferation. Cancerous cells hijack the body’s physiological systems through metabolic reprogramming of the TME. Such reprogramming contributes to tumorigenesis through the activation of biological processes that support cell survival, proliferation, and growth.
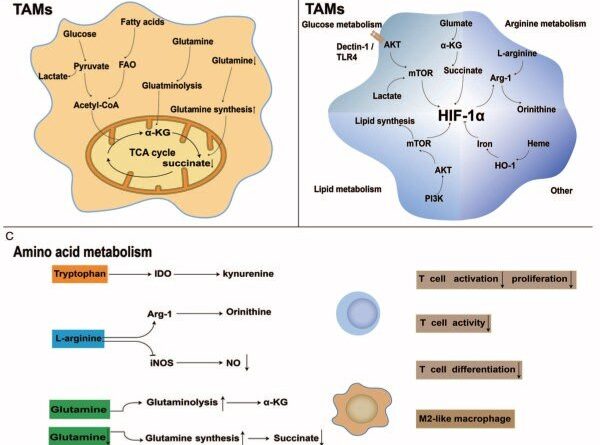
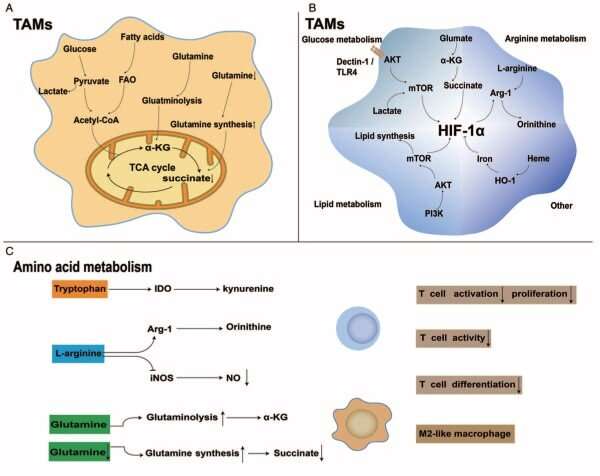
Because of the TME remodeling, TAMs are able to modulate key metabolic pathways involving glucose, lipid, and amino acid metabolism and cause an immunosuppressive TME, thus shielding cancerous cells from the vigilant immune system and enabling their unchecked growth. Owing to the aforementioned reasons, targeting the metabolism-related pathways of TAMs may exert anti-tumor effects. It is therefore important to study TAM-related metabolic targets in the TME.
“TAMs express a pro-tumor phenotype by increasing glycolysis, fatty acid oxidation, cholesterol efflux, and arginine, tryptophan, glutamate, and glutamine metabolism. Previous studies on the metabolism of TAMs demonstrated that metabolic reprogramming has intimate crosstalk with anti-tumor or pro-tumor phenotypes and is crucial for the function of TAMs themselves. Targeting metabolism-related pathways is emerging as a promising therapeutic modality because of the massive metabolic remodeling that occurs in malignant cells and TAMs,” says Dr. Zhang.
TAMs manipulate metabolic pathways in many different ways. For example, enzymes promoting the metabolism of glucose were found to be over-produced in TAMs isolated from patients with pancreatic cancer. TAMs are also known to alter iron metabolism. Because tumor cells require excess iron, TAMs—key sources of iron—release it into the TME, thus increasing its availability to tumor cells.
These processes can be manipulated, though. Targeting metabolism-related pathways has been shown to be effective in suppressing tumors in mice and even in clinical trials. The inclusion of therapeutics like immune checkpoint inhibitors (ICIs) further increases the efficacy of targeting metabolic therapies. ICIs are drugs that blocks proteins called “checkpoints.” These proteins are synthesized by immune cells as well as cancer cells (which imitate our body’s cells and thereby avoid being detected and destroyed by our own vigilant immune system). Clinical evidence clearly suggests that the efficacy of ICIs is improved when therapeutic strategies targeting metabolism-related pathways are included in the treatment plan.
Source: Read Full Article