Microbiome: Scientists highlight role of harmful gut bacteria in fever afflicting cancer patients
An altered gut microbiome is an unexpected cause of fever afflicting many patients undergoing chemotherapy, according to scientists who’ve also discovered that poor appetite during cancer treatment may trigger the biological forces that can likewise adversely raise body temperature.
The domino effect that leads to dangerous fevers in cancer patients is driven by a loss of infection-fighting white blood cells, a condition called neutropenia. Chemotherapy lowers blood neutrophils—white blood cells and key constituents of the immune system—resulting in fever in some, but not all, cancer patients. The new research shines a spotlight on the role of the gut microbiome and how it can promote neutropenic fever.
An interdisciplinary group of researchers at the University of Texas MD Anderson Cancer Center in Houston has uncovered intriguing evidence demonstrating that an increase in a specific species of detrimental bacteria can overwhelm the gut among people receiving chemo. The research adds a tantalizing new dimension of understanding to the role of the gut microbiome among patients undergoing one of the most widely administered forms of cancer care.
“Not all patients with cancer and severe neutropenia develop fever [but] the fecal microbiome may play a role” in complicating patients’ progress, reports Dr. Zaker Schwabkey, of the department of genomic medicine at MD Anderson.
As the lead author of a new analysis on neutropenia and fever in cancer patients, Schwabkey and colleagues highlight a couple of ways that harmful gut microbes can increase as a consequence of chemotherapy.
Concerns about neutropenia and fever are important because an estimated half of people with cancer who are receiving chemotherapy develop some degree of neutropenia. For patients undergoing treatment for leukemia, it’s a common side effect, according to the American Cancer Society.
The Infectious Diseases Society of America defines fever in neutropenic patients as a single oral temperature of 101 degrees Fahrenheit, which is about 38.3 C; or, a temperature of 100.4 degrees Fahrenheit (38.0 C) sustained over a period of one hour. Neutropenic fever in anyone undergoing cancer treatment is considered an emergency because these patients are immune-suppressed and the underlying infection can morph into life-threatening sepsis.
Oncologists also underscore that patients who develop neutropenia are at elevated risk of developing serious, life-threatening infections that are tougher to fight. Vulnerability to infection can be directly traced to not having a sufficient population of infection-fighting neutrophils to kill invasive infection-causing organisms.
The MD Anderson research delved into how cytotoxic chemotherapy can help increase certain gut metabolites, raise the level of deleterious bacteria and diminish the protective mucus lining of the intestines.
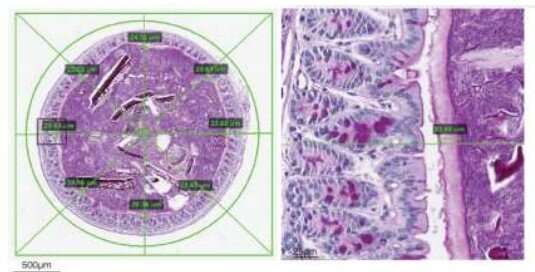
Turning to an animal model in the laboratory, the team discovered that when they transferred the gut microbiota from 119 patients with cancer who developed neutropenic fever to irradiated mice, some of the animals inevitably developed a fever, too.
What the team found when analyzing the gut microbiota of the mice was an excess of mucin-degrading Akkermansia bacteria, the same bacteria in the patients with neutropenic fever. The study of fecal samples confirmed that Akkermansia muciniphila replicates prolifically in the absence of sufficient neutrophils and is linked with subsequent fever. The bacteria are also noteworthy because they are mucin-degrading, which means they actively deplete the protective mucin layer of the intestines.
A total of 63 patients—53%—developed a fever and their fecal microbiome displayed increased accumulation of Akkermansia muciniphila, the same species that grew excessively in the mice.
Reporting in Science Translational Medicine, Schwabkey and collaborators also studied animals that didn’t receive transplants of patients’ gut microbiota. These mice, like their counterparts receiving human gut microbiota were irradiated and treated with chemotherapy. But this second group of animals also had their food intake reduced, which resulted in a compromised intestinal barrier and, surprisingly, led to the excessive growth of A. muciniphila bacteria.
Interestingly, the team found that the bacterial overgrowth could be circumvented with the administration of propionate. This popular food additive is capable of preventing mold formation. As an additive, propionate is found in a wide range of products, from baked goods to energy drinks. Propionate also discourages bacterial growth, which makes it ideal to prevent the growth of Akkermansia muciniphila.
In the mice, targeting their A. muciniphila bacterial growth with propionate or an antibiotic helped preserve the gut mucus layer and reduced inflammation and fever. These interventions suggest possible preventive and therapeutic strategies against neutropenic fever in patients with cancer, the team concluded.
“Treating irradiated mice with propionate or an antibiotic targeting A. muciniphila preserved the mucus layer, suppressed translocation of flagellin, reduced inflammatory cytokines in the colon, and improved thermoregulation,” Schwabkey noted. “These results suggest that diet, metabolites, and colonic mucus link the microbiome to neutropenic fever and may guide future microbiome-based preventive strategies.”
More information:
Zaker I. Schwabkey et al, Diet-derived metabolites and mucus link the gut microbiome to fever after cytotoxic cancer treatment, Science Translational Medicine (2022). DOI: 10.1126/scitranslmed.abo3445
Journal information:
Science Translational Medicine
Source: Read Full Article
