Nearly a third of patient deaths in mental health wards potentially avoidable, according to study
New research suggests close to one in three deaths in inpatient psychiatric care in New South Wales were due to self-harm or potentially avoidable medical conditions.
Almost a third of deaths that occur in mental health wards could be potentially avoidable. That’s the finding of new research from UNSW Sydney, which suggests more needs to be done to improve physical health care access to prevent deaths in people with severe mental illness.
The study, published recently in the Journal of Psychiatric Research, found 471 deaths in inpatient psychiatric wards over a 10-year period in New South Wales (NSW)—141 of which were deemed preventable.
Potentially avoidable deaths are those that could have been prevented through timely and effective medical intervention and should not occur in a well-functioning health care system. While premature mortality in people with mental illness is well-documented, deaths during inpatient psychiatric care have traditionally received little attention.
“The high proportion of potentially avoidable deaths is concerning, and there is a clear need to develop better preventative strategies and improve the overall quality of care for people with severe mental illness,” says Dr. Pramudie Gunaratne, MD, lead author of the study and research fellow at the Department of Developmental Disability Neuropsychiatry, UNSW Medicine & Health.
While every death in a mental health ward in Australia is individually examined, for example, via a coroner’s investigation, the study is the first to systematically investigate all-cause mortality in mental health wards in the country.
“We were originally looking to compare all-cause mortality rates in New South Wales with other states,” Dr. Gunaratne says. “It was surprising to find nothing we could benchmark with as there wasn’t a systematic monitoring process for inpatient deaths during psychiatric care in Australia.”
Physical health a significant cause of death
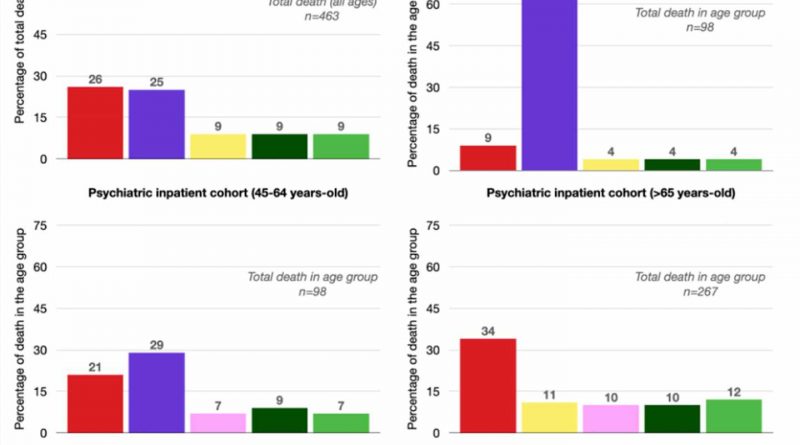
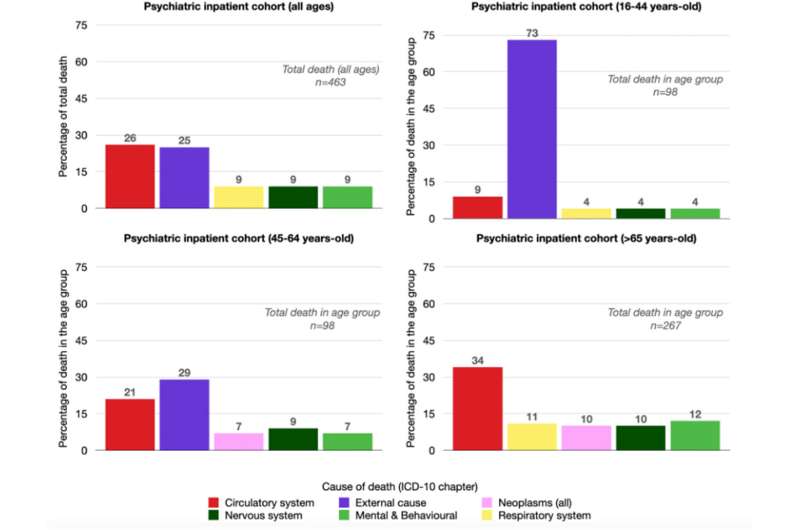
For the study, researchers analyzed a large, linked dataset of mental health admissions in NSW (public and private health care) from 2002 to 2012 to investigate mortality rates and causes of death during inpatient psychiatric care.
Approximately one inpatient death occurred for every 1,000 episodes of inpatient psychiatric care. While the death rate declined over time, there was also an increase in the number of admissions over the 10-year study period.
The leading cause of death was physical health problems, such as issues with the circulatory system, which accounted for 75% of all-cause mortality. Deaths from suicide and accidental death accounted for the remaining 25%.
“Understandably, there is a focus on reducing deaths from suicide in mental health wards; these are an absolute tragedy when they occur,” says Dr. Gunaratne. “But we also know people with mental illness have higher rates of physical health comorbidities—they may be taking medications with metabolic side effects, and can experience stigma and other barriers that limits access to physical health care—all of which may contribute to the significant number of deaths from physical health problems in mental health wards.”
Integrated health care is needed
Dr. Gunaratne says better integrated physical and mental health care may help reduce potentially avoidable inpatient deaths. This encompasses better primary and preventative care in the community to improved access to physical health care in psychiatric wards.
“Unfortunately, managing people with illnesses that span the brain-body divide is incredibly challenging from within systems that traditionally separate mental and physical health care,” Dr. Gunaratne says.
“One of our key recommendations is that patients in inpatient psychiatric care settings have thorough physical health reviews and monitoring while in a ward.
“But it really needs to start with improving access to physical health care in the community to ensure optimal physical health before patients enter an inpatient unit.”
The findings also highlight the need for a coordinated approach to monitoring deaths in mental health wards, including using shared databases and standardized reporting systems.
“Our dataset stopped in 2012, so we simply don’t know how the death rates and causes may have changed over the last decade,” says Dr. Gunaratne. “So, there’s a need for more comprehensive monitoring of inpatient psychiatric deaths across a national and state-wide level.
“Until we have that data, designing the effective interventions we need will be challenging.”
More information:
Pramudie Gunaratne et al, Mortality and cause of death during inpatient psychiatric care in New South Wales, Australia: A retrospective linked data study, Journal of Psychiatric Research (2023). DOI: 10.1016/j.jpsychires.2023.05.043
Journal information:
Journal of Psychiatric Research
Source: Read Full Article