Neutralizing antibodies against SARS-CoV-2 variants induced by homologous and heterologous COVID-19 booster vaccination
Since the beginning of the coronavirus disease 2019 (COVID-19) pandemic in 2019, the causal agent, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has evolved, owing to mutations in the viral genome. This has led to the emergence of many variants classified as variants of concern (VOC) and variants of interest (VOI), per their virulence, transmissibility, and ability to evade immune responses induced via natural infection or COVID-19 vaccination.
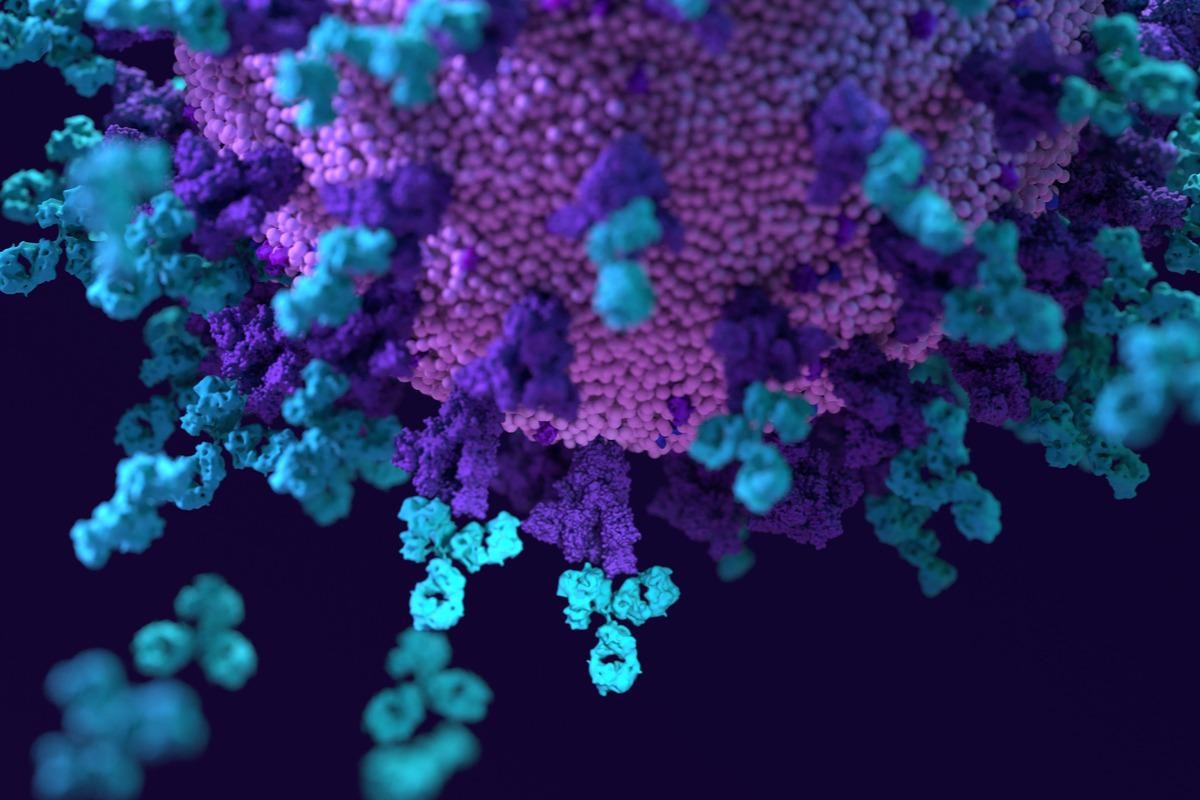 Study: Omicron Neutralizing and Anti-SARS-CoV-2 S-RBD Antibodies in Naïve and Convalescent Populations After Homologous and Heterologous Boosting With an mRNA Vaccine. Image Credit: Design_Cells/Shutterstock
Study: Omicron Neutralizing and Anti-SARS-CoV-2 S-RBD Antibodies in Naïve and Convalescent Populations After Homologous and Heterologous Boosting With an mRNA Vaccine. Image Credit: Design_Cells/Shutterstock
Background
At present, the SARS-CoV-2 variant that is dominantly circulating in many countries across the world is the Omicron variant, which has been classified as a VOC by the World Health Organization (WHO). Scientists have reported that this variant contains a very high number of mutations in the Spike protein. To date, all the available COVID-19 vaccines and therapeutics have been designed against the S protein of the original SARS-CoV-2 strain that emerged in Wuhan, China, in 2019. Therefore, researchers urgently studied the ability of the Omicron variant to escape immune responses generated via immunization or natural infection as well as determined the efficacy of therapeutic antibodies against this variant.
Preliminary studies associated with the Omicron variant have revealed a drastic decrease in antibody reactivity in vaccinated individuals and a general resistance of this variant to most licensed monoclonal antibodies. However, scientists reported that a COVID-19 booster dose could partially restore the neutralization ability against the Omicron variant, but the extent of neutralization differed drastically among the studies. The differential reports might be due to considerable heterogeneity in the population assessed, different neutralization assays used, and lack of calibration with WHO international antibody standards (IS). These studies lacked information about protection estimates against Omicron and other SARS-CoV-2 variants.
Previous studies have provided the essential theoretical support for inferring correlates of protection, which were based on the normalization of neutralizing antibody titers of vaccinated candidates against those who obtained antibodies from sera of convalescent individuals.
A new study
Recently, scientists determined if homologous and heterologous COVID-19 booster vaccination could induce neutralizing antibodies against SARS-CoV-2 original strain and its variants, i.e., the Delta, Beta, and the Omicron variants. They assessed this phenomenon in naïve adults, convalescent adults, and pediatric populations. This study is available online at SSRN.
In this study, scientists focused on identifying tentative cut-offs for large-scale evaluations of immune protection against SARS-CoV-2 and its variants. In this context, they paired live virus neutralization assays with a high-throughput chemiluminescence assay, targeting the receptor-binding domain (RBD) of the spike (S) protein. COVID-19 booster vaccination was performed using the BNT126b2 vaccine. Individuals who received heterologous booster vaccination were primed with the ChAdOx1 nCov19 vaccine. The levels of antibodies in children infected with the Delta variant were assessed 3.5 months after infection. The authors used already published predictive models to determine variant-specific thresholds of protection.
A preprint version of the study is available on Preprints with The Lancet*.
Main findings
In this study, scientists generated data to determine how well immune responses, induced via vaccination or infection, can protect an individual against the Omicron, delta, and beta variants. This study revealed that six months after two doses of the BNT126b2 vaccine, the antigenic mismatch with Omicron was equal to 28x and higher than ever recorded for previous VOCs. Homologous boosting with BNT126b2 vaccine-elicited robust humoral response towards the original SARS-CoV-2 strain as well as its variants including Omicron.
However, a comparable reactivity was not observed when heterologous boosting was applied with BNT126b2, crossing over with the ChAdOx1 nCoV-19 vaccine. Scientists also reported that individuals with mild prior infection with original SARS-CoV-2 strain and subsequent homologous vaccination with BNT126b2 elicited high levels of antibodies but with a moderate breadth of response. Children between 5 and 11 years exhibited minimal neutralizing antibodies against the Omicron variants a few months from infection.
Recent studies have developed models to determine the threshold value for neutralizing antibody titers and anti-spike antibody concentrations associated with protective efficacy against infection with the SARS-CoV-2 original strain. In this study, the authors used these models and determined 90% protection efficiency (PE) of the booster vaccine against SARS-CoV-2 original strain and variants. They reported that the model predicted 34% PE before administering the booster vaccine. Although estimating the duration of the “high protection” status was not the scope of this present study, scientists highlighted that this status was maintained at least 3-5 months post triple vaccination. While dealing with assays, the authors reported the acceptable optimal cut-offs of 2208 BAU/ml for Omicron and 809 BAU/ml for Beta variant.
Key limitations
This study has some limitations, some of which are associated with the predictive model used. One of the limitations is that the study cohort includes only female healthcare workers, whose average age was 49 years. This is the reason why scientists could not observe the broader neutralization ability of booster vaccines across all genders and age groups. Although threshold values for PE against variants were reported in BAU/ml, these values were calculated according to the conversion recommended by the manufacturer, and no information was available regarding the standardization methods that generated the conversion factor.
*Important notice
Preprints with The Lancet publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Pagliari, M. et al. (2022) "Omicron Neutralizing and Anti-SARS-CoV-2 S-RBD Antibodies in Naïve and Convalescent Populations After Homologous and Heterologous Boosting With an mRNA Vaccine", SSRN Electronic Journal. doi: 10.2139/ssrn.4016530. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4016530
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Assay, Children, Coronavirus, Coronavirus Disease COVID-19, covid-19, Efficacy, Genome, Healthcare, Homologous, Immunization, Omicron, Pandemic, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Therapeutics, Vaccine, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
