New care model delivers hepatitis C treatment to most vulnerable
Breakthrough treatments introduced over the last decade have transformed hepatitis C from a chronic and potentially deadly infectious disease into one that can be cured. But these medications have often been beyond the reach of those who are most vulnerable to the virus that causes it: people who inject drugs and lack stable housing.
To address this gap, researchers at UC San Francisco have developed a new model of care that brings medicine to people immediately after their diagnosis. The neighborhood-based, test-and-treat approach was as effective among injection drug users, many of whom were experiencing homelessness, as clinic-based hepatitis C treatment has been for the broader population.
Their study, published in JAMA Network Open, is the first in the United States to evaluate such a program outside a health-care setting. It found that 92% of those who completed the treatment, along with a follow-up blood draw, had undetectable levels of the hepatitis C virus (HCV). Eighty-four percent had sustained virologic response, meaning they were cured three months after treatment.
“Offering hepatitis C treatment at the point-of-diagnosis streamlines care, saving both time and money,” said the study’s first author, Meghan D. Morris, Ph.D., MPH, an associate professor in the UCSF Department of Epidemiology & Biostatistics. “By delivering our ‘one-stop-shop’ model in a non-clinical setting it also tackles the major barrier preventing people who inject drugs and individuals from marginalized communities from accessing curative treatment: stigma.”
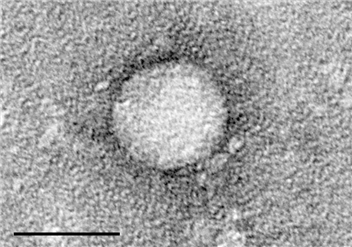
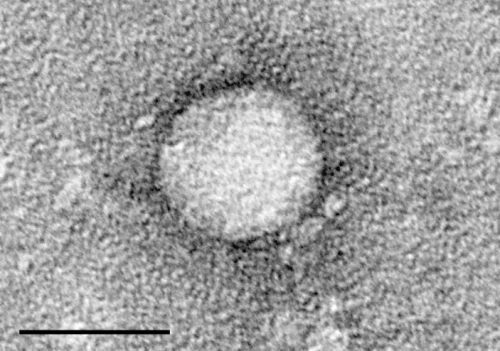
About 2.4 million Americans are living with hepatitis C, an insidious liver disease caused by a virus that is spread through the blood. The disease, which can cause severe liver damage, leads to about 15,000 deaths a year, according to federal statistics. Until the COVID-19 pandemic, HCV killed more Americans than all other reportable communicable diseases.
More than 80% of new hepatitis C infections are associated with sharing needles and syringes used for injecting drugs, and the increasing rate of new cases has corresponded to the growing use of opioids in recent years. The virus can also be transmitted through sex and via childbirth.
New HCV therapies first introduced a decade ago have changed the course of the disease, leading to cures for the vast majority of those who follow the two- to three-month treatment course. Recurrence after treatment is extremely rare—around 1 percent—but it is possible to get reinfected with HCV.
Still, only about a third of patients get treated within a year of being diagnosed with the highly contagious disease, according to the U.S. Centers for Disease Control and Prevention.
“Despite curative treatment, nearly half of people living with hepatitis C are unaware of it, and only a minority of those diagnosed are offered treatment. Our study population is even less likely to be diagnosed and cured because they encounter numerous barriers all along the hepatitis C care cascade, including navigating the health care system and experiencing medical stigma,” said Jennifer C. Price, MD, Ph.D., an associate professor in UCSF’s division of gastroenterology and hepatology, and senior author of the study.
As part of the No One Waits, or NOW, study, UCSF researchers used street outreach to recruit people to get tested at the neighborhood site close to transportation hubs, offering small cash payments as an incentive. They also offered general health information, COVID vaccinations, sterile syringes and hot meals.
The team enrolled 87 people, about 80% of whom were injecting drugs and 61% of whom were experiencing homelessness. Their median age was 48 years old.
They were treated with a combination of sofosbuvir and velpatasvir, which is sold under the brand name Epclusa by Gilead Sciences, a sponsor of the study. Participants received a two-week starter pack of the pills, which are taken daily for 12 weeks. They returned every two weeks after that to pick up more medication, and the study staff had the medication delivered to those who didn’t show up.
Although San Francisco resident Claudette Blueford, 62, tested positive for hepatitis C several years ago, she did not pursue treatment. As someone who uses intravenous drugs and was experiencing homelessness, she explained, it wasn’t a priority.
Blueford initially joined the study to get paid. She only began to appreciate the benefits it could bring to her health once the researchers explained the seriousness of the disease.
None of the participants experienced an adverse event or died. But scarred and collapsed veins from years of drug use prevented a quarter of those in the study from having their blood drawn to see if they were cured. Blueford was among those considered cured.
“It was so easy to get rid of,” she said. “You just take some pills.”
Bulford found stable housing mid-way through the study and has since reduced her drug use.
“You know it’s hard with people on drugs, because they don’t want to listen,” she said, adding that the researchers treated her with kindness and respect. “I started listening to what they were saying. It made sense, and I was in.”
The researchers say the results show the potential of providing hepatitis C test-and-treatment programs at such places as shelters, libraries and food sustenance programs.
The authors noted the current two-step testing process to diagnose hepatitis C, antibody screening followed by RNA testing, remains a barrier, but they hope their findings will encourage point-of-care RNA testing to be approved soon in the U.S.
More information:
Meghan D. Morris et al, Community-Based Point-of-Diagnosis Hepatitis C Treatment for Marginalized Populations, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.38792
Journal information:
JAMA Network Open
Source: Read Full Article