New insights into liver cancer using organoids
Scientists of the Princess Máxima Center for pediatric oncology and Hubrecht Institute in the Netherlands have revealed new scientific insights into the features of fibrolamellar carcinoma (FLC), a rare type of childhood liver cancer.
Their findings, published today in Nature Communications, may help in developing new drug therapies in the future. Mini organs and the ‘molecular scissor’ system CRISPR-Cas9, allowed the researchers to better understand tumor biology and biological consequences of different DNA changes. It also uncovered the probable cell-of origin of one of the FLC tumor types.
Fibrolamellar carcinoma (FLC) is a type of liver cancer, mostly affecting adolescents and young adults. Affecting one in 5 million people per year, fibrolamellar carcinoma can certainly be called rare. The survival rate is still low. In order to change this, new forms of treatment are highly needed.
Novel human organoid models
Dr. Benedetta Artegiani, research group leader at the Princess Máxima Center for pediatric oncology, and Dr. Delilah Hendriks, researcher at the Hubrecht Institute, co-led a new study on fibrolamellar carcinoma by using innovative technologies. This allowed the researchers to better understand the different biological consequences of different mutations found in FLC and to study the biology of the tumors. This new information is needed to understand why the tumors arise, and to identify possible targets for better treatments for the disease.
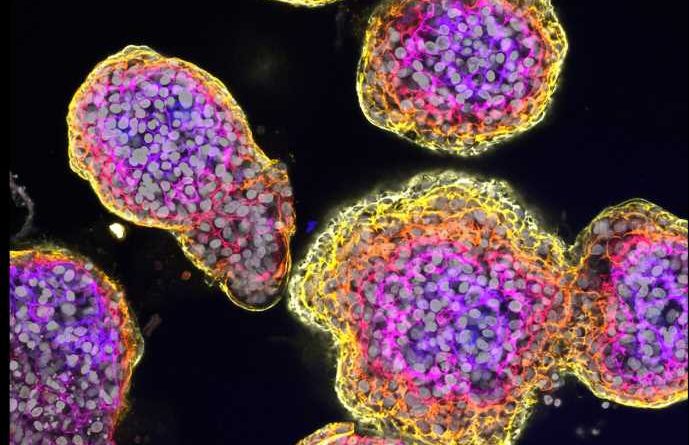
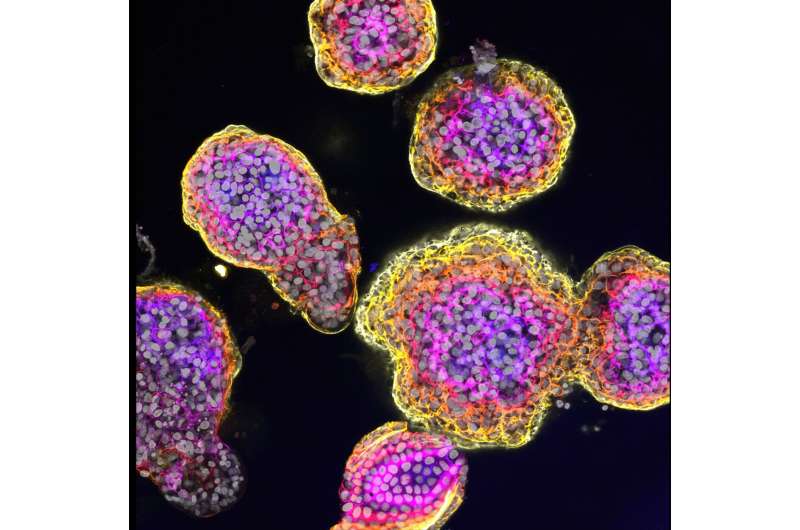
Artegiani says, “We used healthy human liver organoids, mini-livers grown in the lab, in our research. We developed a series of organoids, all with different DNA changes, mutations, that had previously been linked to FLC. We changed the genetic background of the organoids using the DNA modification technique CRISPR-Cas9, that works as a ‘molecular scissor.’ Due to its rarity there is not many tumor tissue available for research. Thanks to this technique we were able to study this tumor type.”
Different genetic mutations underlie different degrees of aggressiveness
Artegiani and Hendriks constructed the liver organoid models by modifying the protein kinase A (PKA) using CRISPR-Cas9. PKA is a complex signaling protein, able to switch other proteins on or off. This ‘protein switch’ is made up of different units, each of them encoded by a different gene. Changing the function of the different units through genetic changes seems to be crucial for the onset of FLC.
The organoids contained the so-called mutant fusion gene DNAJB1-PRKACA. This DNA change is very often found in FLC tumors. Hendriks says, “When reconstructing this mutation in the organoids, we saw that it indeed is able to mirror multiple features of the tumors we see in patients with FLC. Yet, this single mutation caused a rather mild effect on the overall cellular and molecular behavior of the liver cells.”
The situation completely changed when they introduced another set of DNA changes, also found in patients with FLC. Artegiani says, “This second background not only contains a mutation in one of the PKA genes, PRKAR2A, but also in an additional gene called BAP1. In this case, the organoids presented features typical of an aggressive cancer. This suggests that different genetic FLC backgrounds lead to different degrees of tumor aggressiveness.”
Next to this, the greatly enhanced transforming effect caused by the BAP1 and PRKAR2A DNA changes allows the cells to adapt to different environments. This possibly explains the uncontrolled growth of cells during FLC tumor formation.
The researchers concluded that although mutations in the PKA genes are crucial, they might not be sufficient for development of FLC. Hendriks says “These findings open the possibility to look for other factors to occur together with PKA mutations in FLC tumors. This could be potentially exploited for possible future therapies for this form of childhood cancer.”
Uncovering the cell-of-origin in fibrolamellar carcinoma
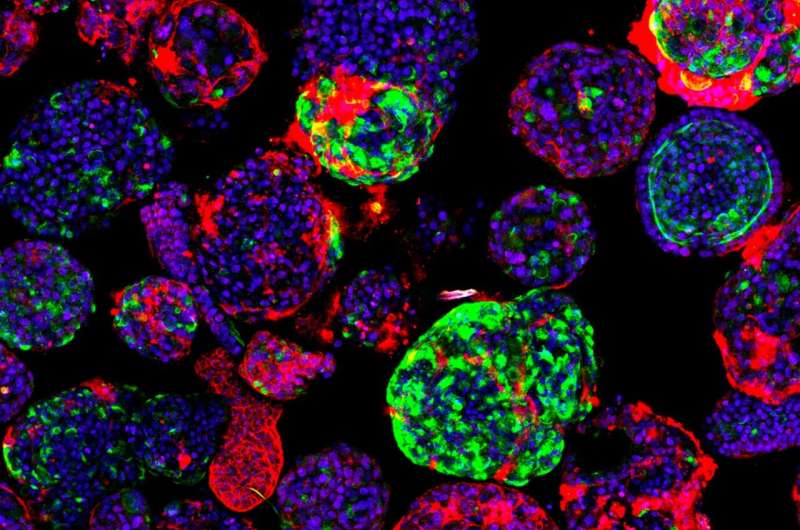
To be able to develop new therapies, it is also essential to understand the biology of the cancer itself. One of the first steps is understanding from which cell type the cancer originates: the cell-of-origin. Understanding the importance of specific gene faults in the initiation of FLC and the original cell could be crucial to understand how the tumor could behave later on.
However, during the study, this turned out to be particularly difficult for FLC. “The main cause is that these tumors present features of both hepatocytes and ductal cells, the two most important cells in the liver. Our organoids showed that the cooperation of PRKAR2A and BAP1 transformed an originally healthy hepatocyte into a ductal cell, with increased cancer stem cell features,” says Artegiani.
“This transformation of a cell type into another one is called transdifferentiation. This is a particular interesting phenomenon that could happen in various tumors, and makes the identification of the cell-of-origin particularly difficult. However, with the use of our models, we were able to uncover the hepatocytes as the probable cell-of-origin.”
Altogether, this study greatly advances the understanding of FLC and paves the way for further research on how to better treat this rare cancer type. The insights in genetic defects could potentially lead to new therapies for children with this disease. And understanding the importance of specific gene faults in the initiation of FLC could in the future also help to better understand tumor heterogeneity and response between patients.
More information:
Organoid models of fibrolamellar carcinoma mutations reveal hepatocyte transdifferentiation through cooperative BAP1 and PRKAR2A loss, Nature Communications (2023). DOI: 10.1038/s41467-023-37951-6
Journal information:
Nature Communications
Source: Read Full Article