New surgical tools with smart sensors can advance cardiac surgery and therapy
Researchers developed a new class of medical instruments equipped with an advanced soft electronics system that could dramatically improve the diagnoses and treatments of a number of cardiac diseases and conditions.
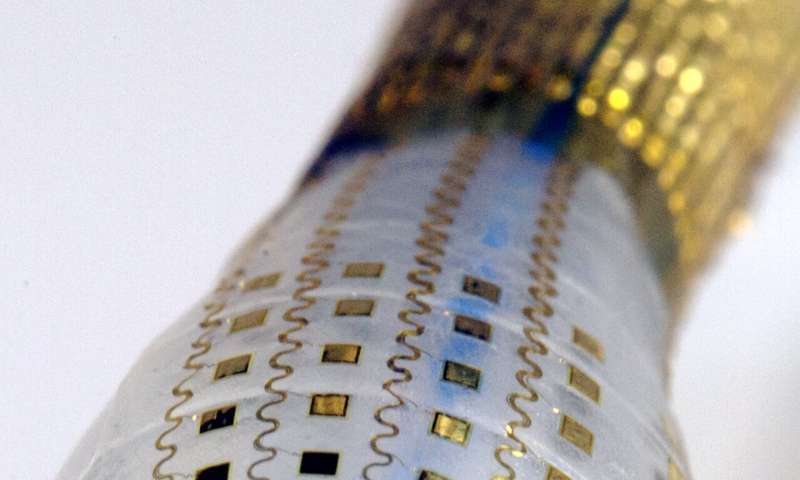
Detailed in a new paper published in the journal Nature Biomedical Engineering, the researchers, led by engineers at the George Washington University and Northwestern University, applied stretchable and flexible matrices of electrode sensors and actuators, along with temperature and pressure sensors, to a balloon catheter system, often used in minimally invasive surgeries or ablations to treat conditions such as heart arrhythmias.
The new system, which conforms better to the body’s soft tissue than current devices, can perform a variety of functions, including: simultaneous in vivo measurements of temperature, force of contact and electrophysiological parameters; the ability to customize diagnostic and therapeutic functions; and real-time feedback. The new system can also dramatically reduce the length of invasive ablation procedures and exposure of patients and doctors to X-ray radiation.
The situation
Many minimally invasive surgeries rely on catheters inserted into the body through small incisions to conduct diagnostic measurements and therapeutic interventions. Physicians, for example, use this catheter-based approach to map and treat irregular heartbeats, or arrhythmias, often by locating and killing or ablating cardiac tissue area which is causing the arrhythmias.
Though widely used in surgery, the current catheter-based approach has a number of drawbacks. The rigidity of today’s catheter devices means they do not conform well to soft, biological tissues, impacting high fidelity mapping of an organ’s electrophysiological signals. Current devices make contact with only a small part of an organ at a time, making it necessary to constantly move a probe around, lengthening medical procedures. Current catheter systems are also limited in the number of functions they can perform, requiring physicians to use multiple catheters in a single ablation procedure.
Additionally, long procedures—for example, to locate and ablate tissues causing arrhythmias—risk exposing both patient and physician to potentially damaging X-rays, as physicians rely on X-ray images during the course of the surgery to guide their catheters.
The benefit
The new class of instruments the researchers developed will allow physicians to acquire a rich set of electrophysiological information and to complete surgeries in shorter times with a single instrumented catheter system.
By outfitting a balloon catheter with advanced organ conformal electronic components, sensors and actuators, the researchers overcame the flaws of current systems. Specific advances over previous systems include:
- Instrumented sensors and actuators in multiplexed array formats can probe the complex nature of tissues, specifically in the beating heart. This will allow, for example, for better localization of sources of lethal arrhythmias causing sudden cardiac death.
- The device’s multilayered and multifunctional architecture with combined diagnostic and therapeutic functions enhances a number of minimally invasive cardiac procedures, including radio frequency or irreversible electroporation ablation—wherein cardiac or nerve cells are ablated, or “burned,” to eliminate sources of arrhythmia—and the delivery of drugs and other biomaterials directly into cells through a process called reversible electroporation.
- Capabilities for real-time feedback control, enabled by simultaneous, multimodal operation of sensors and actuators.
“We have taken new breakthrough materials and fabrication techniques typically employed by the semiconductor industry and applied them to the medical field, in this case cardiology, to advance a new class of medical instruments that will improve cardiac outcomes for patients and allow physicians to deliver better, safer and more patient-specific care,” says Igor Efimov, the Alisann and Terry Collins Professor of Biomedical Engineering at the George Washington University
Source: Read Full Article
