Newer diabetes treatments are understudied in Black populations and may be less beneficial
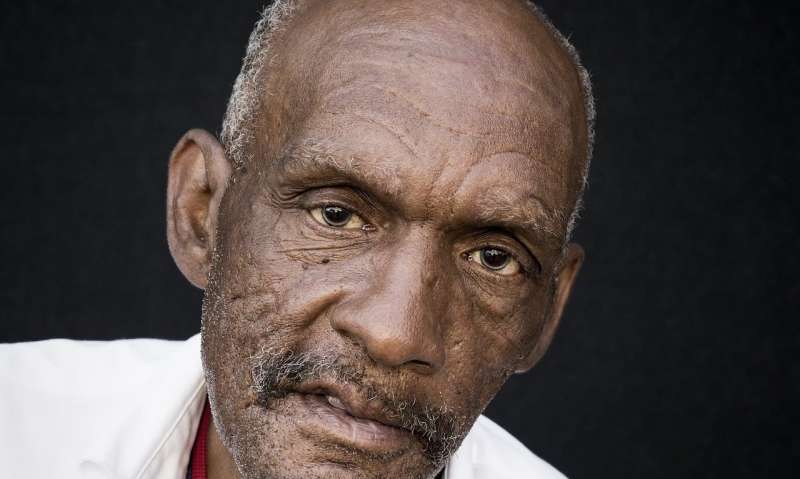
New research analyzing the effects of two drugs used to treat type 2 diabetes indicates a consistent lack of cardiovascular and renal benefits in Black populations. Cardiovascular disease is the leading cause of severe illness and death associated with type 2 diabetes. Renal disease is also a common complication of type 2 diabetes.
The drugs, called sodium-glucose co-transporter 2 inhibitors (SGLT2-Is) and glucogen-like peptide 1 receptor agonists (GLP1-RAs), are some of the newer treatments prescribed to lower blood sugar levels in people with type 2 diabetes.
The research findings, published in the Journal of the Royal Society of Medicine, show that for white and Asian populations, SGLT2-Is and GLP1-RAs have beneficial effects on blood pressure, weight control and renal function, and significantly reduce the risk of severe heart problems and kidney disease. However, the research shows no evidence of these beneficial effects in Black populations.
Researchers at the Diabetes Research Centre at the University of Leicester analyzed the results of 14 randomized controlled trials of SGLT2-Is and GLP1-RAs reporting cardiovascular and renal outcomes by race, ethnicity and region.
Lead researcher Professor Samuel Seidu, Professor in Primary Care Diabetes and Cardio-metabolic Medicine at the University of Leicester, said, “Given the well-documented evidence that Black and other ethnic minority populations are more likely to develop type 2 diabetes and at a younger age, the consistent lack of benefits we observed among Black populations is concerning.
“Minimizing racial and ethnic variations in the cardiovascular and renal complications of type 2 diabetes requires targeted improved access to care and treatment for those most at risk.”
The researchers suggest there are many factors that could have contributed to the lack of evidence of beneficial effects for Black and other non-white populations. Low statistical power due to small sample sizes of these populations may be partly responsible.
“It is quite clear from the current data that some racial/ethnic groups such as Black populations were underrepresented in all the included trials,” pointed out Professor Seidu.
Enrollment in the trials ranged from 66.6% to 93.2% for white populations, 1.2% and 21.6% for Asian populations, and 2.4% to 8.3% for Black populations.
However, the researchers suggest that given the consistent nature of the significant lack of beneficial effects across the majority of outcomes for Black populations, other factors may also be at play.
“Whether the differences are due to issues with under-representation of Black populations and low statistical power or to racial/ethnic variations in the way the body and these drugs interact with each other needs further investigation,” said Professor Seidu. “It is therefore important that prescribers don’t hasten to deny these newer treatments to Black populations on the back of this research.”
More information:
Racial, ethnic and regional differences in the effect of sodium–glucose co-transporter 2 inhibitors and glucagon-like peptide 1 receptor agonists on cardiovascular and renal outcomes: a systematic review and meta-analysis of cardiovascular outcome trials, Journal of the Royal Society of Medicine (2023). DOI: 10.1177/01410768231198442
Journal information:
Journal of the Royal Society of Medicine
Source: Read Full Article
