Not all statins are created equal when it comes to reducing mortality risk in COVID-19 patients
We’ve all recently gotten a crash-course in drug repurposing, thanks to near-daily news reports about efforts to identify existing medicines that could help treat COVID-19 in the early phase of the pandemic. A team of scientists at the Wyss Institute at Harvard University jumped into the fray in the spring of 2020, applying novel computational drug repurposing approaches to confront the COVID-19 challenge.
This early work led to the surprising prediction that a some, but not all, types of statins (drugs that are widely prescribed to lower cholesterol) might protect patients against SARS-CoV-2 infection. In the flurry of clinical studies being published by other scientists studying COVID-19, some found that statins seemed to reduce mortality in COVID-19 patients, while others found no effect—but these studies did not discriminate between different types of statin drugs.
Now, the Wyss team along with collaborators at Stanford University and University of California, San Francisco (UCSF) have confirmed that only a subset of them, including simvastatin (Zocor) and atorvastatin (Lipitor), reduce mortality risk in COVID-19 patients. The team also demonstrated that simvastatin potently inhibited the virus and reduced the production of inflammatory cytokines, while other statins did not.
“This work helps to illuminate the fact that the biomedical community doesn’t fully understand the mechanisms of action of drugs that are very, very commonly prescribed. There’s a lot of work that can be done to study the multiple functions of drugs to discover new uses for existing medications,” said co-first author Megan Sperry, Ph.D., a Postdoctoral Fellow at the Wyss Institute. The research is published in PLOS Computational Biology.
Predicting potency
It has been recognized for some time in the field of statin research that even though all statins target an enzyme called HMGCR to reduce cholesterol, different drugs seem to exert different effects on patients. But the impetus to tease out what exactly those are was lackluster until COVID-19 came along.
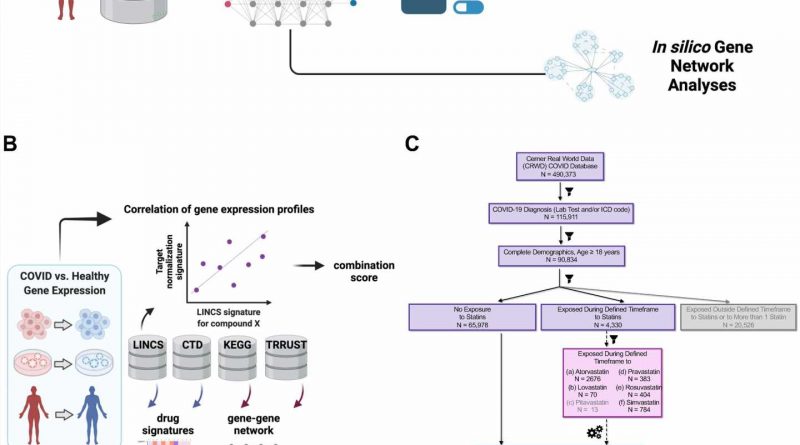
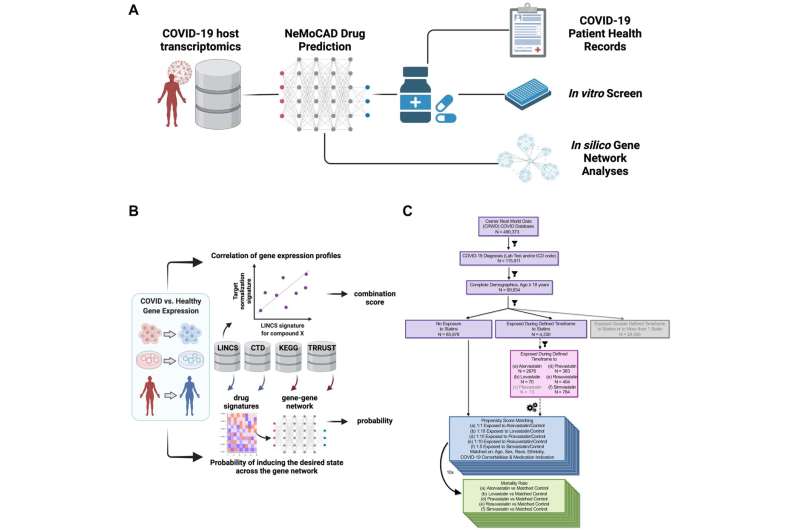
As part of its effort to stem the tide of the pandemic, the United States’ Defense Advanced Research Projects Agency (DARPA) awarded the Wyss Institute $16 million in the spring of 2020 to identify and test FDA-approved drugs that could be repurposed to prevent or treat COVID-19. Statins were among the compounds evaluated by the Wyss team using a computational tool they had developed called Network Model for Causality-Aware Discovery (NeMoCAD).
NeMoCAD uses a network analysis-based algorithm to predict drugs that could revert a diseased gene network back to a healthy gene network; in this case, gene networks found in tissue samples from COVID-19 patients versus those in healthy patient samples. Any drugs that NeMoCAD predicted would be able to convert diseased gene networks into healthy gene networks would then be further tested using cell culture, human Organ Chips, and animal models.
The researchers analyzed 2,436 drugs with NeMoCAD, and noticed that a subset of statin drugs were among those predicted to restore a COVID-19 state to a healthy state, including simvastatin, atorvastatin, pravastatin (Pravachol), lovastatin (Altoprev), and fluvastatin (Lescol). However, only simvastatin and atorvastatin were ranked as highly protective; the others showed a much weaker predicted effect, even though all statins share a common, well-defined mechanism of action against their target.
These observations and similar in vitro experimental data led the Wyss team to conclude that statins varied sufficiently in their effects against SARS-CoV-2 to warrant a deeper dive to determine which individual drugs could potentially treat COVID-19.
Meanwhile, other scientists around the world studying COVID-19 started to publish research showing that patients taking statins seemed to be protected against the worst effects of SARS-CoV-2 infection. But these studies had classified the entire category of “statins” as effective, while the Wyss team knew from their NeMoCAD studies that it was highly likely that only a subset of statins were actually protective.
Co-senior author Richard Novak, Ph.D. reached out to teams at Stanford University and UCSF that had published some of this work on statins, proposing that they collaborate with the Wyss researchers to unravel the distinct effects of specific statins within their dataset.
Novak recognized two features of this patient population that made it especially optimal for further study: people taking statins had similar risk factor profiles (i.e., high cholesterol), and doctors prescribe statins interchangeably, effectively randomizing which patients had received which statin.
One drug comes out on top
Together, the groups performed a retrospective analysis of more than 4,000 patients who were actively taking statins when they became infected with SARS-CoV-2. The results showed that only simvastatin and atorvastatin correlated with significantly increased survival in COVID-19 patients. This confirmed that not all statins have the same effects on the human body, despite their molecular similarity.
Additional in vitro studies in living cells found that only simvastatin strongly inhibited the virus’ ability to infect non-human primate cells; the other statins tested were either ineffective or toxic at the dose required to achieve any effect. Simvastatin also inhibited the infection of human cells with a related coronavirus known as OC43 and reduced the levels of multiple inflammatory cytokines without causing toxicity.
The results from both the patient data and the in vitro studies also largely matched NeMoCAD’s original predictions about which statins would be effective against SARS-CoV-2 infection.
“Thanks to the availability of large amounts of clinical patient data and the Wyss Institute’s multidisciplinary capabilities, we were able to go deeper than previous studies by using multiple models and types of analysis to determine how different statins affect rates of infection and the body’s immune response,” said Novak, who was a Lead Staff Engineer at the Wyss Institute when the research was performed.
“Ultimately, this paper demonstrates how we can combine the diverse tools we have in the lab in a deliberate manner to better understand how drugs work and enable more rapid repurposing for future pandemics or other clinical needs.” Novak is currently the CEO and co-founder of Unravel Biosciences.
The Wyss team is continuing to use this approach to uncover drugs that can be repurposed for various uses, including putting tissues or whole organisms into a state of biological “suspended animation” to extend the amount of time they can survive before getting treatment.
“Drugs are approved for a single use in the human body, but the existence of what we commonly call ‘side effects’ for nearly every medication strongly suggests that these compounds actually affect multiple biological systems,” said corresponding author and leader of the DARPA COVID-19 program, Donald Ingber, M.D., Ph.D. “Studies like this one are a very clear demonstration that off-target effects of FDA-approved drugs can and should be characterized and harnessed in useful ways to address pressing problems in human health.”
More information:
Megan M. Sperry et al, Target-agnostic drug prediction integrated with medical record analysis uncovers differential associations of statins with increased survival in COVID-19 patients, PLOS Computational Biology (2023). DOI: 10.1371/journal.pcbi.1011050
Journal information:
PLoS Computational Biology
Source: Read Full Article