Once a near COVID-free utopia, Australia sees omicron surge

Like millions of others in the most locked-down place on the planet, Melbourne resident Rav Thomas dutifully spent 262 days confined to his home as the COVID-19 pandemic raged. He got vaccinated. And the single father of two found ways to pay the bills as Melbourne’s lockdowns—the longest imposed by any city in the world—battered his entertainment and events company.
Then in October, the city’s restrictions began to lift, along with Thomas’ spirits. His company once again began booking events as Melbourne’s nightclubs and bars reopened.
And then, omicron arrived.
The coronavirus variant has swept across Australia despite its high vaccination rate and strict border policies that kept the country largely sealed off from the world for almost two years. Those measures, which turned Australia into a virtually COVID-19-free utopia early in the pandemic, have garnered fresh scrutiny as the government has battled to deport unvaccinated tennis star Novak Djokovic ahead of the Australian Open. And they have prompted questions from frustrated and fatigued Australians about why their country—which seemingly did everything to stop the spread of of the virus—now finds itself infested with it.
“Tell your population, ‘Stay in your houses, you can’t go past your letterbox after 8 p.m. for days and months on end.’ And then you’re told, ‘OK, we’ve put in the hard yards,'” says Thomas, whose company, Anthem Entertainment, is now facing its 23rd consecutive month of financial loss as bookings once again dry up. “But then here we go again. Again. Again!”

Officially, there are now more than 600,000 active cases across Australia’s population of 26 million, though experts believe the actual number is far higher. The surge, health experts say, is partly due to the coinciding of two events: Politicians who were reluctant to renege on pre-omicron promises that they would relax restrictions such as mask-wearing, and the emergence of the incredibly contagious variant. Faced with the explosion of infections, the government of the most populous state, New South Wales, ultimately backtracked and reimposed mask mandates last month. But by then, epidemiologists say, it was too late.
While deaths and hospitalizations remain relatively low, the vaccines have not stopped the spread of the virus. Australia’s vaccine program—which has resulted in around 80% of the total population having at least one jab—also began later than many other Western countries, leaving much of its population yet to qualify for a booster.
“Vaccination alone isn’t good enough,” says epidemiologist Adrian Esterman, chair of biostatistics and epidemiology at the University of South Australia. “We were doing so well, until New South Wales decided it didn’t want to go into lockdown.”

Esterman has urged politicians to enforce mask-wearing and social distancing, and to improve ventilation in schools, particularly as students prepare to return after the southern hemisphere summer break. Children between the ages of 5 and 11 only became eligible for the vaccines this month.
“We haven’t got enough vaccines for youngsters,” says Esterman, who previously worked for the World Health Organization. “We know how to keep schools safe: First, get kids and teachers vaccinated, make sure ventilation is very good and you get the kids to wear masks. Do we do that in Australia? No.”
Though Australia’s high vaccine uptake has prevented an even worse crisis at stressed hospitals, Australian Medical Association President Dr. Omar Khorshid acknowledged it was difficult to watch Australia plummet from its position as a poster child for COVID-19 containment.

“It is certainly frustrating to see our case per head of population rate sort of getting toward the highest in the world in New South Wales, for instance, when we were at the lowest in the world not that long ago,” he said. “It’s a little unfortunate that the opening up of the country coincided almost perfectly with the omicron outbreak starting around the world.”
In recent months, the government has pivoted from its longstanding “COVID-zero” approach to a “live with it” approach, leaving many Australians confused.
“Omicron has changed everything,” Prime Minister Scott Morrison said this week. “My government is for keeping Australia open and pushing through.”
The policy whiplash also caught the health system off guard. Lines for PCR tests are often hours long, results take days, and a lack of rapid antigen tests has left sick Australians scurrying from store to store hunting for the kits.

Sydney resident Rodney Swan recently found himself among the hordes hunting for rapid tests. The 77-year-old’s granddaughter is ill, and her family has been isolating at home for days as they await the results of their PCR tests.
“If you do get a test that’s a PCR test, then you wait ages,” Swan says. “You can’t get a rapid antigen test. My daughter can’t get boosters for her children.”
Swan is frustrated by what he views as the government’s jumbled messaging, and is stunned by the skyrocketing case numbers.
“These are numbers that you get in England,” he says. “I’ve got friends in London, because I lived in London, and I sense the smirk that they have now looking at Australia.”
Australia’s slow start to its booster program has left the population vulnerable to omicron, and has also increased the chances that its omicron wave will not decline as rapidly as other countries, says epidemiologist Dr. Nancy Baxter, head of the Melbourne School of Population and Global Health at Melbourne University.
Australia’s politicians appear worried that any new restrictions will anger the public, Baxter says. But they can still help slow the spread by providing Australians with a limited number of free N95 masks and rapid tests, she says.
“We could manage the wave, but there’s no political will to do so,” Baxter says.
Fury and fear prompted former Australian human rights commissioner Chris Sidoti to pen an opinion piece for the Sydney Morning Herald this week, detailing the terror he felt when his two immunocompromised grandchildren become ill with COVID-19 after Christmas, two weeks before they were eligible for the vaccine. Both children have been in and out of the hospital since then.
Sidoti blames his grandchildren’s plight on the government. Why, he asks, wasn’t the government prepared with adequate supplies of rapid tests before the PCR system became inevitably overwhelmed? And why did the New South Wales premier roll back restrictions such as mask-wearing in November, before young children were eligible for vaccines and before most adults were eligible for boosters?






“We have gone wrong from day one because our politicians are not prepared to learn and to prepare,” Sidoti said in an interview. “People have stopped listening because there’s no consistency, there’s no credibility and there are no answers.”
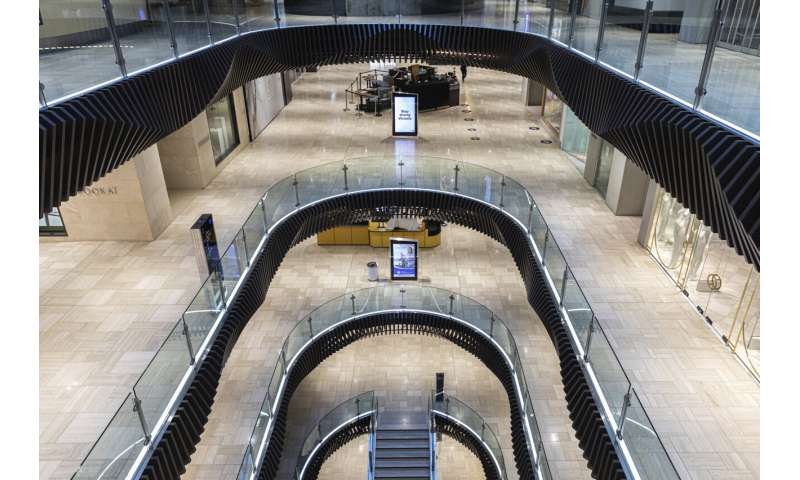
Though policymakers seem averse to further lockdowns, the omicron outbreak has prompted many Australians to stay home anyway, leaving small business owners worried about their companies’ survival.
“People are quite broken,” says Zara Madrusan, who owns several bars and restaurants in Melbourne. “We are basically in some kind of self-imposed lockdown. No one is going out, but there’s no protection for us, there’s no advice for us, there’s no financial support available. So we’re just supposed to muddle through.”
For Thomas, whose company is facing a deluge of event cancellations, the state’s decision this week to shut down indoor dance floors in hospitality and entertainment venues was another gut punch. He wonders what of his once-vibrant city will be left when this all ends.
Source: Read Full Article
