PCPs and Knee OA: When to Keep Treating, When to Refer
Primary care providers (PCPs) play a key role in helping patients with knee osteoarthritis (OA) maintain the best quality of life possible as long as possible.
With no cure or reliable treatments to prevent arthritis or to halt its progress, PCPs guide patients on over-the-counter medications, exercise, diet and nutritionist consultation, and physical therapy to lessen pain, slow degeneration of the joints, and avoid surgery if possible.
“Osteoarthritis is a very common and difficult-to-treat disease that is easily overlooked or written off by busy clinicians and not given the attention and time it deserves,” Matlock Jeffries, MD, clinical assistant professor of medicine at the University of Oklahoma Health Sciences Center in Oklahoma City, told Medscape Medical News. “The most important advice I have for PCPs is to remain engaged with their patients who have osteoarthritis.
“However, I recommend that PCPs refer any patient they do not feel comfortable managing to a provider who specializes in recognizing and treating osteoarthritis,” he added. “Rheumatologists in particular can rule out alternative diagnoses that are sometimes misconstrued as osteoarthritis, including rarer autoimmune diseases; and they can properly diagnose unusual osteoarthritis subtypes.”
Mitigation Strategies, No Cure
The prevalence of osteoarthritis increased to around 528 million people worldwide in 2019 and is expected to continue to rise, the World Health Organization reports. Almost 75% of people with the condition are older than 55 years, and over half are female. The most common joint affected is the knee, with a global prevalence of 365 million.
“With lack of exercise, knee OA worsens over time and the joint becomes more unstable,” Sean M. Drake, MD, a medical director of complex primary care at Henry Ford Health in Detroit, said. “Exercising the muscles around the knee helps strengthen the joint. Non-weight-bearing exercises, pool exercises, aerobics, resistance training, stationary bicycles, and elliptical machines are all good for knees. In moderate to severe knee osteoarthritis, a cane or a knee brace can be of benefit.”
Drake encourages his patients with knee OA to exercise and lose weight and to get any comorbidities, such as diabetes, hypertension, heart failure, or chronic obstructive pulmonary disease, under control, especially if they will need surgery. “In overweight patients, losing 5% to 10% of body mass greatly improves knee osteoarthritis pain,” he said.
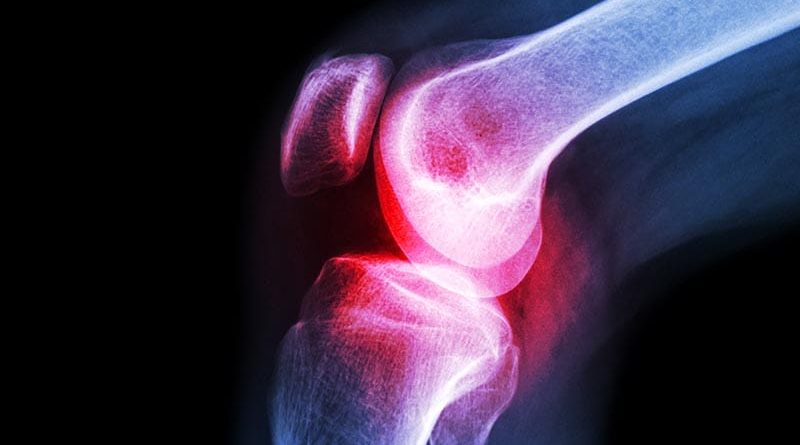
He has had success with showing his patients x-ray or MRI images of a normal knee and comparing them with images of their own damaged joint.
“Seeing patients in the office frequently, offering encouragement, and setting goals ― starting with only 10 minutes of exercise a day and building from there ― can have incremental benefits,” said Carrie Louise DeLone, MD, an internal medicine specialist and medical director of primary care at UPMC Central Pennsylvania in Harrisburg.
Monitor Meds
“Readily available over-the-counter medications help with pain and inflammation, but if used incorrectly, they can cause side effects on other organs, like the kidneys or liver,” cautioned Elizabeth Klag, MD, clinical associate professor in the Department of Orthopaedic Surgery at the University of Michigan in Ann Arbor. “PCPs can monitor for these side effects.”
Nonsteroidal anti-inflammatory drugs are the first-line drugs for these patients, but their utility for the elderly and for those with certain chronic conditions is limited, owing to the high risk of bleeding and kidney damage. Duloxetine and gabapentin have been shown to be effective. Capsaicin, while effective, can cause skin irritation, DeLone said.
“Evaluating patients for depression and social determinants of health that can impact pain is important,” she added. “Long-term pain has not been improved with narcotic pain medications, and the risks for addiction and overdose make them unacceptable. Intrarticular steroid injections are done routinely in PCP offices and can be quite effective.”
Although no good data on complementary treatments for knee OA are available, Drake said, glucosamine chondroitin probably causes no harm. Mind/body interventions, such as tai chi and yoga, strengthen muscles, improve breathing, and may give patients a more positive outlook on their condition.
“Tai chi and possibly curcumin, the active ingredient of turmeric, are likely to help in some way, evidence suggests,” said rheumatologist David T. Felson, MD, MPH, professor of medicine at Boston University Chobanian and Avedisian School of Medicine. “Glucosamine and chondroitin do not work. Acupuncture probably works no better than sham acupuncture, but needles may be therapeutic for pain.”
Most complementary and alternative treatments show little if any evidence of effectiveness in treating OA, said Jeffries. Drugs improve symptoms but do not reduce the likelihood of progression. And newer injectable therapies, such as platelet-rich plasma or intra-articular stem cells, are expensive and have not been rigorously tested.
Helping Patients Stick With Treatment Is Key
Patients can join online exercise classes through apps and videos on YouTube and other websites, including those of the American Association of Hip and Knee Surgeons, the Arthritis Foundation, and the United Kingdom charity Versus Arthritis. Silver Sneakers offers online and in-person gym classes to qualified adults with disabilities and those aged 65 and older.
“However, patients must always be cautious about putting too much stock in osteoarthritis treatment websites,” Jeffries warned. “The purveyors of expensive supplements and therapies are focused on profits rather than patient outcomes.”
When to Refer
Despite a PCP’s optimal treatment and a patient’s compliance, the joint continues to degenerate. When pain compromises quality of life, it’s time to refer the patient to a specialist to discuss their options and the risks and benefits of surgery, Sean Ryan, MD, adult reconstruction surgeon and assistant professor in the Division of Orthopaedic Surgery at Duke Health in Durham, North Carolina, advised. “Sports medicine or orthopedics specialists are useful to refer to when considering injection therapy.”
PCPs need to be open to the possibility that the patient may not have OA, Felson noted. For example, they may instead have gout, pseudogout, or another form of inflammatory crystal-induced arthritis.
“PCPs should consider a rheumatology referral if the patient has signs of inflammatory arthritis, such as multiple involved joints, skin changes, and elevated serum rheumatologic markers. Rheumatologists can manage disease-modifying antirheumatic drugs,” said Klag. “If the patient has mechanical symptoms such as clicking, popping, or locking, they should be referred to an orthopedic surgeon to evaluate for a meniscus tear.”
Patients who experience worsening of stiffness, loss of motion, or knee deformity should be referred to a surgeon promptly, because delays can make the procedure more challenging and can increase the risk of complications, she added.
Barriers to Care
Body mass index (BMI) and comorbidities can be barriers to surgery; some insurance companies and surgeons place upper limits on BMI for undergoing surgery, Drake said.
“For knee replacement, patients should have BMI below 40, hemoglobin A1C under 7.5 if diabetic, and be nonsmokers,” Ryan said. “Our PCP colleagues are in a great position to improve these medical comorbidities before arthritis becomes severe enough to need surgery.”
PCPs can help patients overcome time and transportation challenges by having them enroll in at-home exercise programs. For patients who need immediate specialist care, Klag suggested that PCPs request specialists to squeeze them into their schedules.
“One of the biggest barriers knee osteoarthritis patients encounter is a general feeling by many physicians that nothing can be done about osteoarthritis, so it may not be worth diagnosing,” Jeffries said. “Nothing could be further from the truth.”
Recognizing the condition early helps patients mitigate its effects on their lives, he added. “We have strong evidence that decreased physical activity, particularly due to knee osteoarthritis–related pain, can increase the risk for other diseases, including cardiovascular disease, hypertension, hyperlipidemia, and diabetes. Controlling osteoarthritis symptoms should be a cornerstone of effective management and prevention of these other problems.”
Promising Research in the Pipeline
Despite the lack of targeted treatments for OA, Jeffries said the future holds promise.
“Do not give up,” he said. “Knee osteoarthritis is very difficult to treat, particularly because we do not yet have any disease-modifying antiosteoarthritic drugs. Several drugs that show promise in regrowing cartilage and reducing pain are in late-stage clinical trials, so seek out osteoarthritis specialists, particularly those involved in osteoarthritis research, who may direct your patients to promising trials.”
Jeffries, Drake, DeLone, and Felson report no relevant financial relationships. Klag had a consulting relationship with Enovis within the past 3 years; Ryan is a consultant for Zimmer Biomet, DePuy Synthes, and Total Joint Orthopaedics.
Lorraine L. Janeczko, MPH, is a medical science journalist in Atlanta.
For more news, follow Medscape on Facebook, X, Instagram, and YouTube.
Source: Read Full Article