Pilot study for T-cell lymphoma finds adding epigenetic drug to standard chemotherapy is effective
Nearly 90% of patients with an aggressive subtype of non-Hodgkin lymphoma had their cancer go into remission in a small phase 2 clinical trial testing a treatment aimed at making chemotherapy more effective, according to Weill Cornell Medicine and NewYork-Presbyterian investigators.
The clinical trial, whose results were published May 4 in Blood, included 17 patients with a type of blood cancer called peripheral T-cell lymphoma with T-follicular helper phenotype (PTCL-TFH), also known as angioimmunoblastic T-cell lymphoma. Fifteen of them (88.2%) had complete responses after a several-month course of treatment, which combined a standard four-drug chemotherapy regimen known as CHOP with another drug called azaciditine. Patients with PTCL-TFH have tumors that typically bear excessive clusters of gene-silencing marks called methylations on their DNA—marks that azacitidine removes.
“The treatment shows promise for this T cell lymphoma subtype, and we look forward to seeing how it performs in a larger clinical trial,” said study lead author Dr. Jia Ruan, a professor of clinical medicine and a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine and an oncologist at NewYork-Presbyterian/Weill Cornell Medical Center.
The study was a collaboration involving multiple investigators at Weill Cornell Medicine, including Drs. Peter Martin, John Leonard, Leandro Cerchietti, Giorgio Inghirami, Olivier Elemento, and Ari Melnick. Investigators from Memorial Sloan Kettering, Washington University School of Medicine, Moffitt Cancer Center and BostonGene Corporation also contributed to the study.
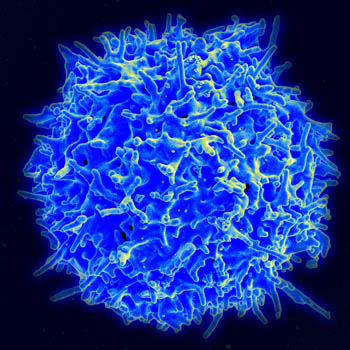
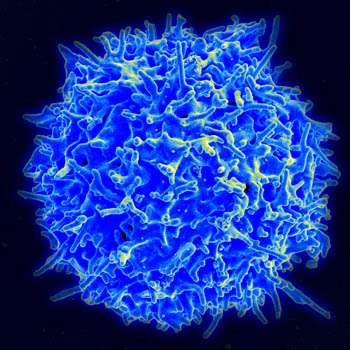
Lymphomas arise from immune cells, mostly B cells and T cells, whose malignant overgrowth leads to the swelling of lymph nodes. These cancers are newly diagnosed in approximately 90,000 people in the United States annually. PTCLs, which account for several thousand of these cases, are relatively hard to treat successfully, and have an estimated five-year survival rate of only 20 to 30%.
A standard initial therapy for most lymphomas is a four-drug chemotherapy regimen (CHOP) that is usually delivered in six three-week cycles. Researchers have been looking for ways to enhance the effectiveness of this treatment for PTCL and other forms of lymphoma that tend to have poor outcomes.
Combining standard chemotherapy with azacitidine is a promising strategy that is now being tested in various settings. A small study led by Dr. Martin and published last year found that the combination therapy was effective in producing complete response rates in patients with certain aggressive B-cell lymphomas.
Azacitidine, which is currently approved by the U.S. Food & Drug Administration for the treatment of myelodysplastic syndrome and some leukemias, works to remove gene-regulating marks on DNA called methylations. Many aggressive cancers harbor dense patches of these DNA marks—hypermethylations—which are thought to enhance tumor survival by silencing growth-restraining and DNA-repair genes.
In the new study, Dr. Ruan and her colleagues examined the effectiveness of the combination in PTCL patients with the TFH subtype, since PTCL-TFH tumors typically show DNA excessive methylation marks as well as mutations in one or more methylation-regulating genes.
The study included 20 evaluable PTCL patients, 17 of whom had the TFH subtype based on genetic tests of their tumors. All but one had advanced PTCLs of stages III-IV. The rate of complete responses at the end of azacitidine-plus-standard chemotherapy treatment was very high: Three-quarters (15/20) of the patients showed complete responses, and all were PTCL-TFH patients—implying a complete-response rate of 88.2% for this subgroup. Although there was no placebo or standard-treatment comparison group, end-of-treatment complete response rates for PTCL patients treated with standard chemotherapy-only, such as CHOP-based regimens, are usually in the 30-40% range, said Dr. Ruan.
The median follow-up time for the patients was 21 months, allowing the researchers to estimate two-year progression-free survival rates of 65.8% for all 20 patients, and 69.2% for the 17 PTCL-TFH patients. Side-effects were comparable to what is normally seen in standard chemotherapy treatment.
These results are consistent with the idea that adding azacitidine to standard chemotherapy is safe and more effective for PTCL-TFH patients, Dr. Ruan said.
The researchers are now working with colleagues across the country investigating azacitidine-plus-standard chemotherapy in a randomized clinical trial in a group of more than 150 PTCL patients of different subtypes, scheduled to be completed by 2026.
More information:
Jia Ruan et al, Multicenter Phase 2 Study of Oral azacitidine (CC-486) plus CHOP as initial treatment for peripheral T-cell lymphoma, Blood (2023). DOI: 10.1182/blood.2022018254
Journal information:
Blood
Source: Read Full Article