Researcher identifies potential cause of ‘long COVID’
Even though the COVID-19 public health emergency classification will expire this spring, the lingering effects of the pandemic remain. A constant puzzle to solve since the first year of the pandemic has been “long COVID,” a condition in which those infected with the virus have symptoms that linger months or even years after they have cleared the initial infection.
“Long COVID is estimated to affect one out of every five people who get COVID,” says Brent Palmer, Ph.D., associate professor of allergy and clinical immunology at the University of Colorado School of Medicine. “It’s described as persistent symptoms that last longer than four weeks post-initial infection. Those symptoms can include chest pain, cough, shortness of breath, brain fog, and fatigue.”
The virus that lingers
Palmer has a theory as to why long COVID—also known as post-acute sequelae of COVID, or PASC—is happening: viral reservoirs that linger in the body, causing the immune system to become overactive in its efforts to eradicate them.
An HIV researcher who became interested early in the potential causes of long COVID, Palmer initiated a study in 2020, looking at a group of 40 patients who had been infected with COVID-19. Twenty cleared the virus completely, and 20 went on to develop PASC. Working with CU pulmonologist Sarah Jolley, MD, who runs the UCHealth Post-COVID Clinic for PASC patients, Palmer collected blood and stool samples from both sets of patients, looking for COVID-19-specific T cells that remained active in the body after the initial COVID infection was gone.
“We took these blood cells, and we incubated them with little parts and pieces of the virus. Then we looked at the frequency of two types of T cells—CD4 and CD8—that respond by producing cytokines,” Palmer says. “The cells that responded to the viral parts were specific for SARS-CoV-2.
“We found a very pronounced high frequency of cytotoxic CD8 T cells in the individuals with PASC,” he adds. “These responses were up to 100 times higher in the PASC group than in the individuals who didn’t have long-term, persistent symptoms.”
Palmer, who also studies HIV infection, was astonished to see that a few people six months out from their initial infection had nearly 50% of their T cells directed against COVID-19.
“That’s an amazingly high frequency, much higher than we typically see in HIV, where you have ongoing viral replication all the time,” he says. “These responses were in most cases higher than what we see in HIV.”
Lung connections
Palmer’s study, published in 2022 in the journal PLOS Pathogens, compares the frequencies of COVID-19-specific T cells and inflammatory markers with lung function in patients who had either pulmonary PASC or resolved COVID-19.
“Because we received these patients from the pulmonary PASC clinic run by Dr. Jolley, we had access to pulmonary function data,” he says. “Patients would come in, they would say, ‘Hey, I have had this persistent cough or shortness of breath for the last six months,’ and she would run them through a pulmonary function test to determine how well their lungs were functioning.”
Correlating his blood test data with Jolley’s pulmonary data, Palmer found an inverse correlation between pulmonary function and the frequency of COVID-19-specific T cells in the blood.
“The higher the frequency of COVID-specific T cells in the blood of that individual, the worse their pulmonary function tests were,” he says. “That showed a really strong connection between these T cells that were potentially driving disease and an actual readout of disease, which was reduced pulmonary function. That was a critical discovery.”
Increased immune response
The results led Palmer and his research team to theorize that PASC symptoms are being driven by the immune system, which is ramping up inflammation in response to the COVID virus that remains hidden in the body post-initial infection.
“We think it’s an overexaggerated immune response that’s causing the problem,” he says. “What we hypothesize is that there’s residual virus somewhere in the body, but it’s not detected by a nasal swab. It has been shown that individuals who died of severe acute COVID had virus all over their body. When they do autopsies on these individuals, they can find virus in the brain, the kidney, the lung, and the gut.”
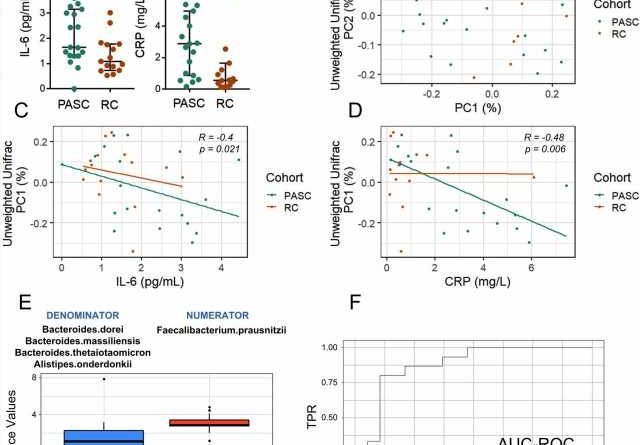
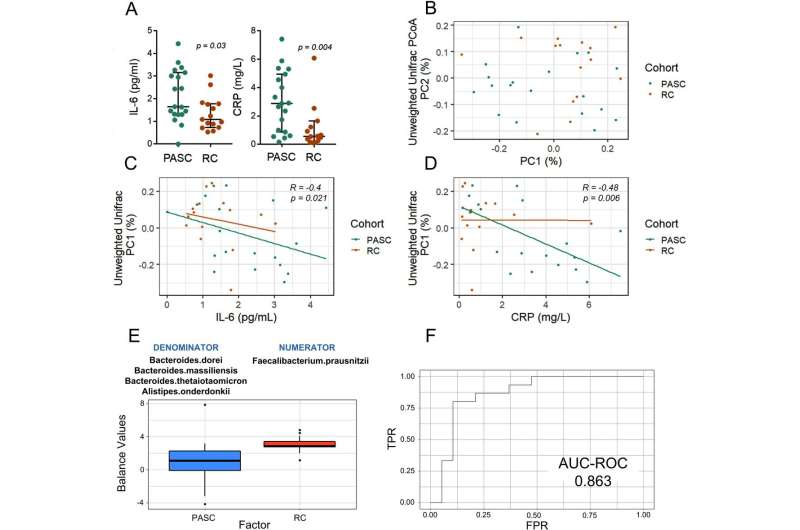
A subsequent PASC study, published in January in the journal Gut and led by Palmer and Catherine Lozupone, Ph.D., associate professor of biomedical informatics, examines data from the stool samples taken from the PASC patients in his study. It shows that the composition of gut bacteria in the stool of individuals with PASC is associated with elevated inflammation markers in the blood, suggesting that there is an association between gut microbiome and systemic inflammation in PASC.
How antivirals could help
Both studies, Palmer says, suggest that an antiviral medication such as Paxlovid could be an effective treatment for PASC.
“There have been studies in individuals with long COVID that have shown that vaccination causes a modest decrease in symptoms,” he says. “If you vaccinate them, you bump up their immune response even more, maybe you get a better antibody response, you root out these viral reservoirs, and that leads to reduced symptoms. Other studies have shown that giving patients Paxlovid can suppress viral replication, and once the viral application is suppressed, the virus-specific immune response will drop off.
“Some of the early data from these studies, especially the Paxlovid study, suggests that suppressing the virus using an antiviral medication might be a treatment for long COVID,” he continues. “It also supports the idea that maybe there is residual virus hanging out somewhere that we haven’t been able to access. Our research suggests that virus is still being produced in hidden reservoir in some individuals long after they’re testing negative with a nasal swab.”
More information:
Valdirene Leao Carneiro et al, Inflammation-associated gut microbiome in postacute sequelae of SARS-CoV-2 points towards new therapeutic targets, Gut (2023). DOI: 10.1136/gutjnl-2022-328757
Journal information:
PLoS Pathogens
,
Gut
Source: Read Full Article