Researchers leverage cell self-destruction to treat brain tumors
Glioblastoma is the most common type of brain tumor in adults. The disease is 100% fatal and there are no cures, making it the most aggressive type of cancer. Such a poor prognosis has motivated researchers and neurosurgeons to understand the biology of tumors with the goal of creating better therapies.
Dominique Higgins, MD, Ph.D., an assistant professor in the Department of Neurosurgery, has heeded the call. Higgins and a team of researchers at Columbia University have found that glioblastoma tumor cells are particularly sensitive to ferroptosis—a type of cell death that can be triggered by removing certain amino acids from the diet.
“First, we found that when we take away certain amino acids in animal models that the glioblastoma cells are more likely to die by ferroptosis,” said Dr. Higgins. “Secondly, we found that removing these amino acids makes our drugs a lot more effective at inducing ferroptosis in cancer cells.”
Their findings were published in Nature Communications.
Ferroptosis is an iron-dependent type of “programmed cell death” or a biological process that causes cells to “self-destruct” on command. Our bodies don’t need to kill cells unless absolutely necessary, so the process is tightly controlled by certain biological mechanisms. However, researchers are only now beginning to comprehend the process because ferroptosis was recognized only a decade ago.
“The recent discovery of ferroptosis adds to the excitement of it all,” said Higgins, who is a member at the UNC Lineberger Comprehensive Cancer Center. “It is really a rapidly growing body of research, and we are finding that it’s a very important for a lot of biological processes, and not just in cancers.”
Every cell has certain safety features to keep it from going through ferroptosis in an unpredictable way. Two amino acids, cysteine and methionine, are critical for preventing the process from starting in cells. We typically pick up these amino acids through our diet.
Therefore, Higgins’ research team decided to focus their efforts on these components.
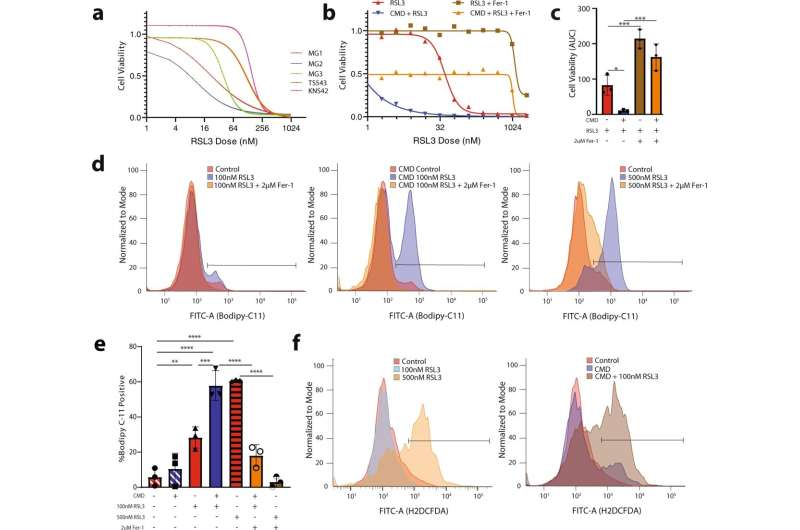
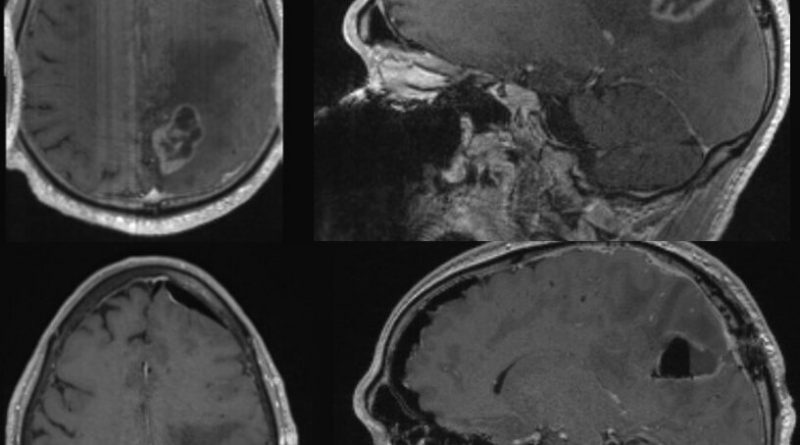
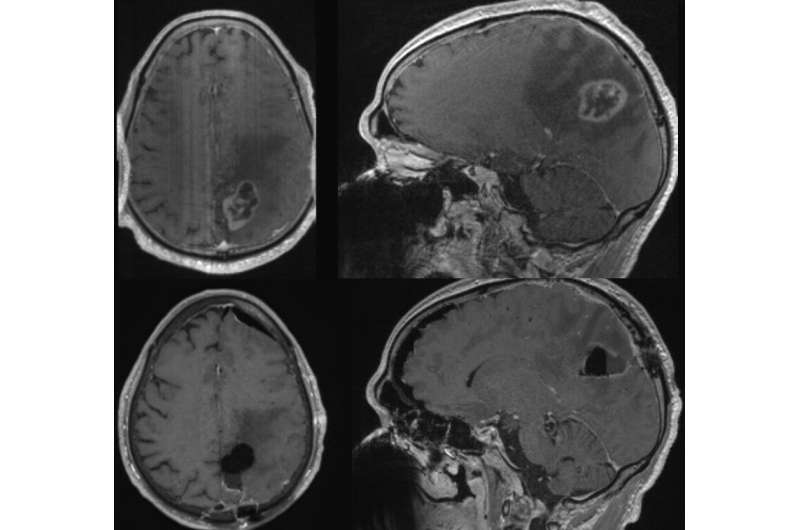
By depriving animal models of cysteine and methionine through a customized diet, they found that the glioblastoma cells were significantly more likely to die via ferroptosis. They also found that the diet made their chemotherapy drugs more apt at initiating programmed cell death, meaning that very low doses were able to achieve a more potent effect than before. Ultimately, the animal models had improved survival after going on the diet.
“Now, we need to find a way to eliminate those components through dietary needs, while still maintaining energetic requirements that a patient may have, especially a cancer patient, who has different requirements than the average patient,” said Higgins.
Having proven that the diet is effective in animal models, Higgins is working with colleagues at UNC Lineberger to develop a clinical trial for patients with glioblastoma. He plans to put patients on the diet prior to surgery to understand how it effects the body and the tumor. Once he removes the tumor from the brain, he will analyze it to see how well the tumors responded to the diet.
This type of diet has also shown to be very effective in sarcoma, lung cancers, and pancreatic cancers, so there is hope that this diet can be used to put some extra umph behind chemotherapy and/or surgery to remove tumors throughout the body.
Higgins is also working with Shawn Hingtgen, Ph.D., professor of pharmacoengineering and molecular pharmaceutics in the UNC Eschelman School of Pharmacy and associate professor in the Department of Neurosurgery, to study the brain’s response to treatment in a more natural setting.
Hingtgen is the overall grant PI for Project Brainslice, a multi-institutional effort to test neurological therapies using tumor samples grown on slices of brain tissue. Higgins maintained that this is a better way to study treatment response than simply observing it in a plastic dish.
Project Brainslice is just one of the many different research tools that researchers have at their fingertips here at UNC’s School of Medicine.
“We have a lot of different research tools unique to UNC, and it is one of the main reasons that I wanted to come to UNC,” said Higgins, who joined UNC Neurosurgery in the fall of 2022. “Just in terms of the ability to study a clinical problem in an accurate animal model, it is one of the few places in the country that has like an established setup to do that.”
More information:
Pavan S. Upadhyayula et al, Dietary restriction of cysteine and methionine sensitizes gliomas to ferroptosis and induces alterations in energetic metabolism, Nature Communications (2023). DOI: 10.1038/s41467-023-36630-w
Journal information:
Nature Communications
Source: Read Full Article