Signaling between cancer and mesothelial cells promotes ovarian cancer tumorigenesis, immune evasion
Ovarian cancer is the fourth-leading cause of cancer mortality among women and is characterized by late detection, extensive metastasis and poor prognosis.
One reason that treating this disease has been so challenging is that tumors often become resistant to chemotherapies, and generally respond poorly to immunotherapies.
While much of the research on overcoming resistance and efforts to develop new therapies have focused on the cancer cells, it has often ignored the many other cell types within the tumor. Indeed, cancer cells have the ability to reprogram the cells around them to nurture the tumor and help evade the patient’s immune system.
One of these cells is the mesothelial cell, which represents the point of first contact of ovarian cancer cells during peritoneal metastasis.
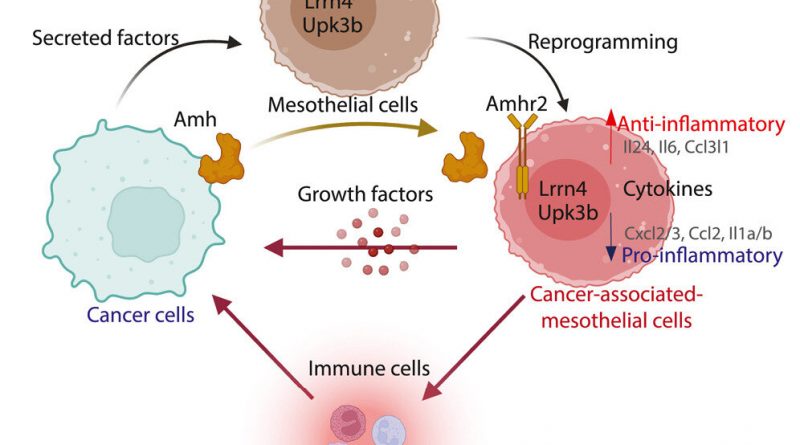
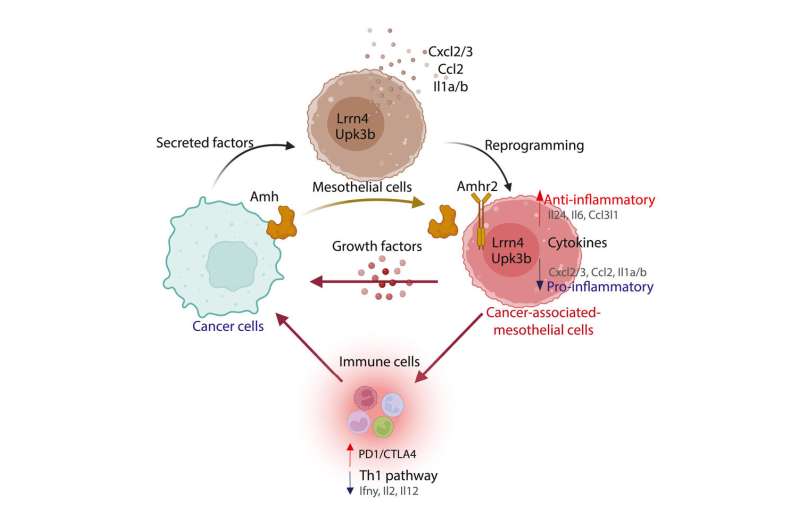
In a new study published in Cell Reports, a research team shows how cancer cell reprogram these mesothelial cells into cancer-associated-mesothelial cell, which then promote the growth of the tumor. Importantly, the researchers identify one of the signals, a hormone called Anti-Müllerian hormone, which is used by cancer cells reprogram and control mesothelial cells.
They show that disrupting this signal slows the growth of the tumor and helps the immune system overcome some of the tumor’s defenses suggesting it may represent a new target in ovarian cancer.
Findings
The study contributes to a new area of research regarding the origin and function of mesothelial cells in the ovarian tumor microenvironment. It demonstrates how cancer cells reprogram normal mesothelial cells into cancer-associated mesothelial cells (CAMC) that have a pro-tumoral function.
At the heart of this reprogramming is the reactivation of an important developmental hormone signal, in the form of the anti-Mullerian hormone (AMH), and its receptor AMHR2.
While AMHR2 had long been assumed to be expressed by cancer cells, the researchers found that instead cancer-associated mesothelial cells are the tumor cell types that carry this receptor, and that ovarian cancer cells produce its ligand, AMH.
Clinical implications
The study reveals that cancer cells use AMH to control cancer-associated mesothelial cells, by modulating their production of growth factors that promote tumor growth and cytokines that help cloak the tumor from the immune system.
This new understanding presents exciting possibilities for therapeutic strategies that aim to neutralize the AMH signal from cancer cells or target the AMHR2 on mesothelial cells to potentially inhibit tumor growth and restore immune response.
Next steps
Currently there are no therapeutic strategies targeting cancer-associated mesothelial cells. This work supports the notion that they may represent a new therapeutic target in ovarian cancer.
But importantly, because mesothelial cells represent the first point of contact of most solid tumor metastasizing in the abdomen, therapeutic approaches that specifically target cancer-associated mesothelial cells could lead to improved treatment outcomes for other cancers.
Furthermore, the identification of AMHR2 as a potential biomarker for cancer-associated mesothelial cells will facilitate future studies on this cell type across these other solid tumors.
Given the intense focus in developing new treatments for women’s health targeting AMH and AMHR2, there is a unique opportunity to repurpose some of these new therapies for the treatment of ovarian cancer, and perhaps improve response to existing immunotherapies.
More information:
M. Chauvin et al, Cancer-associated mesothelial cells are regulated by the anti-Müllerian hormone axis, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.112730
Journal information:
Cell Reports
Source: Read Full Article