Stem cells may help identify new schizophrenia drugs

- Excessive inflammation and aberrant immune system activity in the brain can have severe consequences, including the development of psychiatric and neurodegenerative disorders.
- People with schizophrenia have higher levels of the immune protein C4 in their brains and C4 variations are linked to an increased risk of developing the condition.
- While therapies that reduce C4 levels and inflammation in the brain may benefit schizophrenia patients, none are currently available.
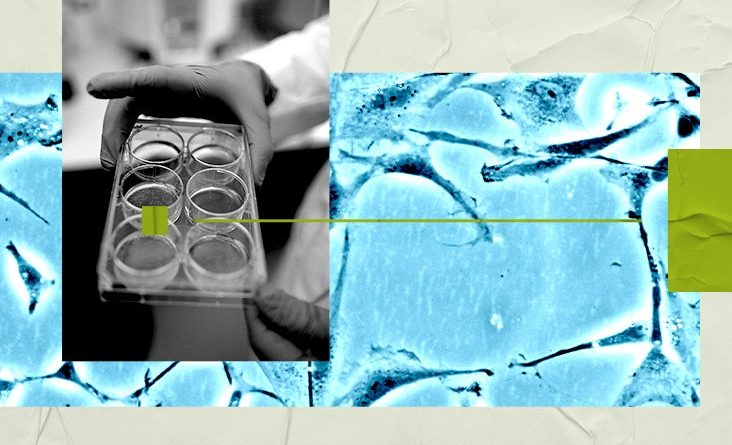
- Now, Harvard University researchers have developed a technique to produce large quantities of C4-secreting human astrocytes from stem cells, promising a new avenue for developing effective treatments.
In a new study, published in Stem Cell Reports, researchers highlight how various genetic differences have previously been associated with a higher risk of schizophrenia.
These differences affect a protein called complement component 4 (C4), which is more active in the brains of people with schizophrenia.
To develop effective drugs for lowering C4 levels, the researchers devised a method to create large quantities of C4-secreting human astrocytes from stem cells.
Astrocytes are cells in the brain that play an important role in connecting brain cells together and removing unnecessary connections. They are part of the brain’s immune system and secrete the C4 protein.
The brains of people with schizophrenia also tend to have fewer connections between certain brain cells. Some researchers think that C4 might be involved in removing these connections.
However, the exact way that C4 is related to schizophrenia is not fully understood.
Producing astrocytes to test medicines
In this new research, the team developed a way to make large volumes of astrocytes and tested different drugs to see if they could affect C4 production.
To study C4 and astrocytes, the researchers used a special technique to make human astrocytes from stem cells in the lab.
The team screened 464 drugs and identified a small group of approximately 20 that reduced C4 secretion from astrocytes. They found some drugs that could control C4 and also predicted other ways to control it.
These drugs were effective in both healthy astrocytes and those derived from schizophrenia patients’ stem cells.
The study presents new opportunities for examining inflammatory responses and their regulation in human astrocytes and provides a platform for identifying potential therapeutic drugs in large-scale screening efforts.
Dr. Louis Cona, the medical director at DVC Stem who was not involved in this research, told Medical News Today that this study “is quite significant as it presents a novel method for generating a specific type of brain cell, called astrocytes, from pluripotent stem cells.”
“Pluripotent stem cells can differentiate into any cell type within the human body, including brain cells,” Cona said. “The researchers have devised a technique that efficiently directs these pluripotent stem cells to become astrocytes, vital in supporting and safeguarding our neurons, the primary communicators within the brain.”
The implications of this research are far-reaching as it not only enhances our understanding of brain function and astrocyte interactions with other brain cells but also enables the rapid and consistent production of astrocytes. This facilitates a more efficient and detailed investigation of these cells.
Dr. Louis Cona
Understanding brain physiology
Cona explained how this research can help us better understand the complex functions of our brains.
“Gaining more knowledge about the brain can improve mental health care, educational strategies, and our overall understanding of human behavior,” he said.
The study’s findings may pave the way for repurposing existing drugs for CNS indications. The identified pathways and regulators may help develop more effective and targeted therapies for conditions like schizophrenia, Alzheimer’s disease, and other neuroinflammatory disorders.
Dr. Louis Cona
Potential implications for patients and the public
“By creating astrocytes from pluripotent stem cells, scientists can study how these brain cells function and interact with other cells in the brain. This can help us learn more about how our brains work and understand and treat brain-related diseases,” Cona explained.
“This research could lead to new treatments and therapies for brain disorders or injured patients. For example, studying astrocytes might help us figure out how to protect neurons, which could help people recover from brain injuries or slow the progression of certain neurodegenerative diseases,” he added.
Dr. Omotola Ajibade, a psychiatry resident and APA/APAF Diversity leadership fellow who also not involved in the study, agreed, telling MNT that “this was a very ambitious project.”
“We’ve known for some time that inflammation plays a significant role in mental health. In recent years, we’ve seen the release of immunologics for treating conditions like Alzheimer’s. Among other things, this study helps to identify other inflammatory pathways that are likely involved in some mental illnesses. Understanding these pathways will greatly aid future research in drug development,” Ajibade said.
“While these results are certainly remarkable, they won’t have any immediate effect for the general public. However, if research in this area continues, it could open a whole new class of medications that we can use to treat conditions like Schizophrenia and Alzheimer’s dementia. [The authors] were very measured in their report and I don’t want to overstate their findings. While some of the compounds they used are already on the market for other diseases, I’m not sure that they’ve been tested specifically for treating neurocognitive disorders. It would be interesting to see how these results would shape up in clinical trials.”
Dr. Omotola Ajibade
Cona notes that this research “delves into the role of protein C4, which is secreted by astrocytes. This protein has been associated with various brain disorders. By elucidating the function of C4, researchers may develop new therapeutic approaches for individuals suffering from brain disorders linked to this protein.”
In conclusion, Cona said, “the excitement surrounding this paper stems from its potential to significantly advance our understanding of the human brain and contribute to developing novel treatments for brain-related disorders.”
“Moreover, it highlights the extraordinary potential of pluripotent stem cells and their applications in human health and scientific knowledge,” he added.
Source: Read Full Article