Study suggests spermidine could help to treat advanced non-alcoholic fatty liver disease
A team of scientists led by Duke-NUS Medical School have identified an important pathway that gets disrupted in the advanced form of non-alcoholic fatty liver disease known as non-alcoholic steatohepatitis (NASH)—and intervening with a naturally-occurring compound known as spermidine partially fixes the problem.
Non-alcoholic fatty liver disease, an umbrella term for a range of liver conditions affecting people who drink little to no alcohol, is the most prevalent metabolic liver disorder worldwide, affecting 25% of all adults globally. In Singapore, non-alcoholic liver disease affects four in 10 adults.
NASH results when the disease progresses and there is inflammation and scar tissue formed in the liver; it is associated with cardiac and kidney disease and malignancies outside the liver. Publishing in Nature Communications, the scientists say understanding how spermidine alleviates the pathological features of NASH could help in developing drugs to treat the condition.
“Currently, there is no pharmacological therapy for NASH, with several drugs showing only limited efficacy in clinical trials, so there is an urgent need to better understand the molecular mechanisms that underlie it,” said the study’s first author Dr. Zhou Jin, Senior Research Fellow with the Cardiovascular & Metabolic Disorders (CVMD) Program at Duke-NUS Medical School, Singapore.
Dr. Zhou, senior author Professor Paul Michael Yen from the CVMD Program, and their colleagues in Singapore, the U.S., the U.K. and China first studied liver enzymes involved in a specific pathway in people who were healthy or had non-alcoholic fatty liver disease. They next carried their studies over to a preclinical model of NASH.
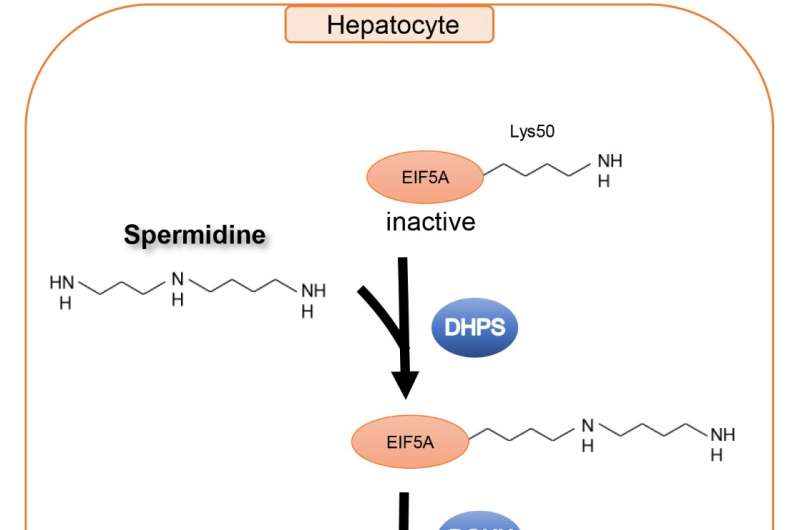
They found a molecular pathway that was disrupted by the condition. Put simply, NASH leads to the reduction of an enzyme, called deoxyhypusine hydroxylase, that is necessary for attaching the hypusine residue from spermidine to a critical protein involved in translating genetic code from RNA onto protein, called EIF5A.
Disruption of the pathway decreased the synthesis of proteins for the cell’s energy powerhouse, called mitochondria. It also decreased mitochondrial activity and fatty acid metabolism.
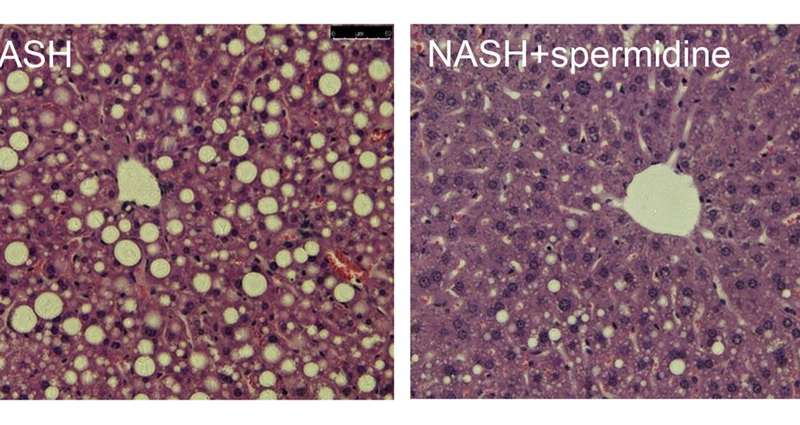
The scientists next added a naturally-occurring compound called spermidine to the cell cultures and preclinical model. They observed increased fatty acid metabolism and improved mitochondrial function. There was also less liver inflammation and scar tissue formation associated with NASH.
“Our findings that the dysregulation of mitochondrial protein synthesis can be rescued by spermidine provides novel mechanistic insights, a therapeutic target, and potential prevention agent for managing non-alcoholic fatty liver disease,” said Prof Yen.
“Basic scientific research proves its value by enabling new discoveries and avenues of research for conditions that have otherwise confounded clinicians,” Professor Patrick Casey, Senior Vice-Dean for Research at Duke-NUS. “There are still many steps before these findings can be translated to humans—nonetheless, the work led by Professor Yen and his lab continues to push the boundaries of what we know about the condition, to better inform how we can effectively treat it.”
Source: Read Full Article
