The long term effects of COVID-19
A recent Monash University study has found six months after recovering from COVID-19 critical illness, one in five people had died, and almost 40 percent of survivors had a new disability.
Led by Professor Carol Hodgson, the study looked at COVID-19 critical illness across Australia between March 6 and October 4, 2020, measuring mortality, new disability and return to work in people who had been admitted to intensive care units.
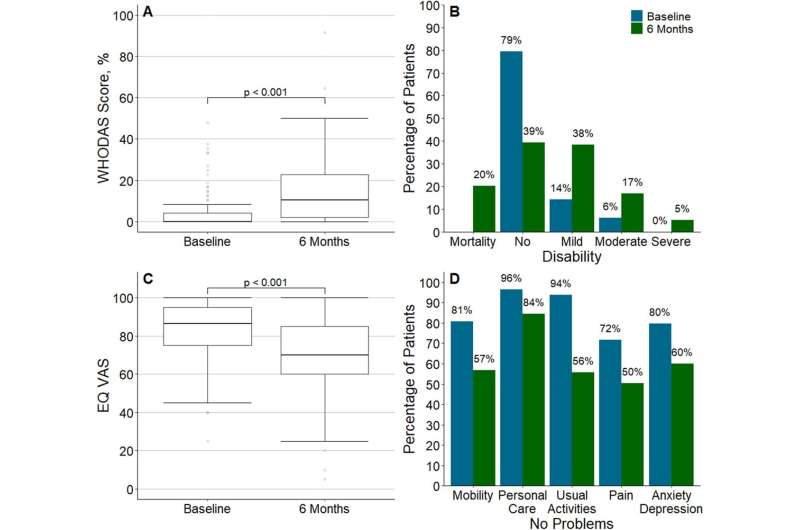
At six months, 43 of the 212 (20.3 percent) eligible patients had died, and 42 of the 108 (38.9 percent) surviving patients who responded to the study reported a new disability.
The study found 71.3 percent of surviving patients reported persistent symptoms such as shortness of breath, loss of strength, fatigue, headaches and loss of sense of smell and taste after recovering from the critical illness.
There was also a significant decrease in health-related quality of life across all domains, but particular participants reported new problems with mobility (33.9 percent), usual activities (43.2 percent) and pain (34.2 percent), as well as cognitive impairment (33.3 percent), and one fifth (20 percent) reporting anxiety (20.2 percent), depression (20 percent) and/or PTSD (18.4 percent). More than one in 10 survivors were unemployed due to poor health.
The findings are published in Critical Care today.
Professor Hodgson is Head of the Division of Clinical Trials and Cohort Studies in the School of Public Health and Preventive Medicine and Deputy Director, Australian and New Zealand Intensive Care Research Centre, Monash University.
The study was embedded in the Short Period Incidence Study of Severe Acute Respiratory Infection trial (SPRINT-SARI) and was conducted at 30 intensive care units across Australia.
With a median age of 61, 58 percent of participants were male with comorbidity of diabetes or obesity. Fifty-seven percent received mechanical ventilation.
“Because COVID-19 is a new disease, the impact on long term outcomes in survivors is still emerging; however these findings suggest that patients should be screened at hospital discharge for new functional impairments, as the burden of new disability after critical illness with COVID-19 represents an urgent public health problem,” Professor Hodgson said.
Sherene, a study participant and healthcare worker from Victoria, spent over a month in the hospital, including 16 days in a coma, departing the hospital in August 2020. Still is not well enough to return to work, and says the ongoing emotional and physical impact of COVID-19 has been frustrating to deal with.
“This virus has aged me 30 years, I am consistently reliant on family assistance to do even the simplest of tasks like cooking and household chores. Stretching to reach the bottom of the washing machine is too much,” Sherene said.
Source: Read Full Article
