Thrombectomy comparable to medical management for strokes, finds study
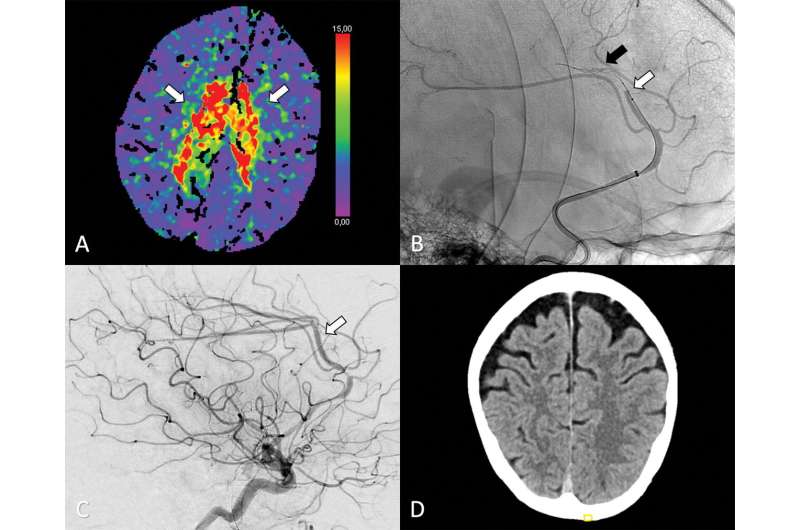
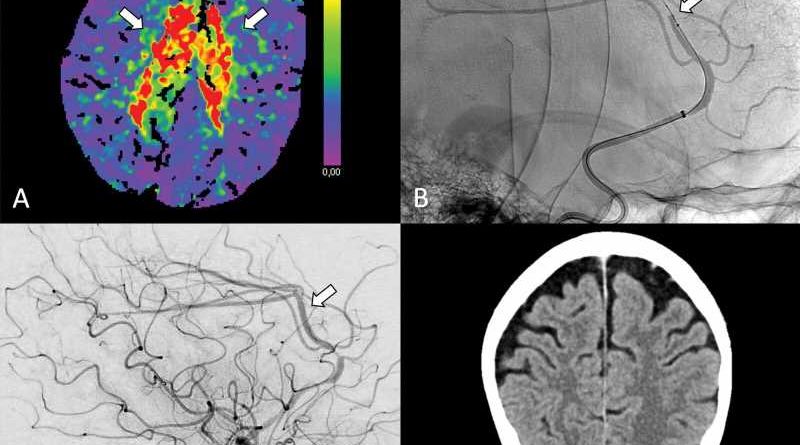
A surgical procedure called thrombectomy is a safe and feasible treatment option for a rare type of stroke, according to a study published in Radiology.
Thrombectomy is commonly performed to remove blood clots from brain arteries. It is often done to treat strokes arising from blood clots in the larger arteries that supply blood to the brain. When done promptly, thrombectomy can sometimes be more successful than clot-busting drugs in mitigating long-term damage to the brain.
Recent advances in technology have made it possible to perform thrombectomy in some of the narrower vessels in the head—vessels like the anterior cerebral arteries that arise from the internal carotid artery. However, evidence supporting a potential benefit of thrombectomy for these vessels remains unknown.
As part of the ‘Treatment fOr Primary Medium vessel Occlusion Stroke’, or TOPMOST trial, researchers in Germany compared thrombectomy with medical treatment in 154 patients. The patients all had primary isolated anterior cerebral artery medium vessel occlusions, or obstructions.
The patients underwent thrombectomy or best medical treatment, which typically involves medications to dissolve the clot and reduce blood pressure. In some cases, patients may receive intravenous thrombolysis, the introduction of clot-busting drugs to the bloodstream or directly to the site of clot.
The researchers assessed early outcome, or outcome within the first 24 hours after treatment, and longer-term functional outcome. They also looked at safety with a focus on bleeding in the brain and death.
The results showed that thrombectomy was a safe and technically feasible option. Within the first 24 hours after treatment, thrombectomy patients had similar outcomes to those who received best medical treatment alone with or without intravenous thrombolysis. Longer term, both groups had similar clinical and functional outcomes. Mortality rates were similar in both groups.
“Based on our study, both treatment options appear to be effective and safe,” said study lead author Lukas Meyer, M.D., from the Department of Diagnostic and Interventional Neuroradiology at University Medical Center Hamburg-Eppendorf in Hamburg, Germany.
“The overall results of the study are consistent with a growing body of literature suggesting that thrombectomy may have a role in the treatment of this type of stroke. Eligible patients should therefore be randomized to ongoing prospective trials whenever possible.”
Dr. Meyer emphasized that the type of blockages his team studied are rare, and all the centers involved in this study were tertiary stroke centers with a high level of expertise in these kinds of interventions.
Selection of patients for thrombectomy remains a key issue, Dr. Meyer said, especially when patients are not eligible for randomization in a designated trial.
“As we anticipate an increasing number of patients with medium vessel occlusions being treated with thrombectomy, age and eloquence of symptoms in particular are factors that should be considered when making treatment decisions,” he said. “Ultimately, the results of ongoing randomized trials will provide further insight into this subgroup.”
Dr. Meyer plans to conduct further analysis of a subgroup of these patients to gain a deeper understanding of procedural and clinical outcomes. He also wants to identify potential surrogate markers that can predict clinical course.
“By focusing on this specific patient population, we hope to further advance our knowledge and improve patient outcomes,” he said.
More information:
Lukas Meyer et al, Thrombectomy versus Medical Management for Isolated Anterior Cerebral Artery Stroke: An International Multicenter Registry Study, Radiology (2023). DOI: 10.1148/radiol.220229
Journal information:
Radiology
Source: Read Full Article