Unexpected cognitive deteriorations in epilepsy
In severe epilepsies, surgical intervention is often the only remedy—usually with great success. While neuropsychological performance can recover in the long term after successful surgery, on rare occasions, unexpected declines in cognitive performance occur. Researchers at the University of Bonn have now been able to show which patients are at particularly high risk for this.
Their findings have been published in the journal Annals of Neurology. They may help identify affected individuals for whom surgery should be avoided. Instead, new treatment prospects are emerging for these patients.
An epilepsy disorder cannot always be controlled with medication. In such cases, sufferers should seek advice as to whether surgery is an option. During the procedure, surgeons selectively remove damaged brain tissue from which seizures originate. This often provides a complete cure for the patients.
“Surgery has revolutionized the treatment of severe epilepsies,” explains Dr. Juri-Alexander Witt, neuropsychologist at the Department of Epileptology at the University Hospital Bonn. “However, with epilepsy surgery, there is always a risk of cognitive decline. That said, long-term studies have shown that brain performance can recover in the long term after successful surgery.”
Unexpected drop in performance months after surgery
However, in a small proportion of sufferers, unexpected drops in performance do not occur until months or years after the surgery. “We wanted to know the reason behind this,” says Annika Reimers, a doctoral student at the Institute of Neuropathology in Prof. Albert Becker’s research group.
The researchers were helped by the University Hospital Bonn’s extensive experience in epilepsy surgery: They were able to draw on brain tissue samples that had in some cases been taken decades ago. “We analyzed a total of 24 samples from men and women who had been diagnosed with serious cognitive decline months or even years after surgery,” Reimers explains.
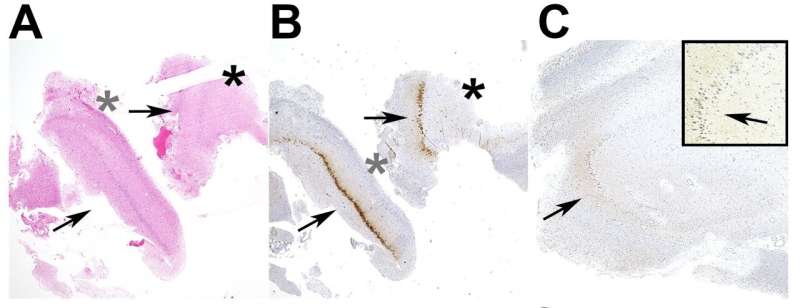
In the course of this, the researchers came across a striking finding: In those affected, the removed tissue was damaged by secondary disease at the time of surgery—either through inflammation or incipient Alzheimer’s dementia-like. “With these pre-existing conditions, the body’s defenses are particularly active,” says Becker, who is also a member of the Transdisciplinary Research Area (TRA) “Life and Health.” “It’s possible that the trauma of the surgical procedure further stimulates the immune system in the brain to attack healthy brain tissue.”
Tests provide guidance on when surgery should be avoided
The researchers now plan to study samples from other epilepsy centers to corroborate their finding. The results may help identify affected individuals for whom surgery should be avoided. “We currently have various diagnostic methods at hand that we can use for this purpose,” says Dr. Juri-Alexander Witt.
For instance, all patients complete an extensive battery of psychometric tests prior to surgery to determine their cognitive performance. When considered together with brain scanner images and the examination of cerebrospinal fluid by means of a lumbar puncture, some of the results already allow conclusions to be drawn about concomitant diseases.
“If such tests indicate inflammation or the onset of neurodegenerative disease, entirely new treatment options emerge, such as anti-inflammatory pharmaceuticals, which may make surgery unnecessary,” Becker says.
More information:
Annika Reimers et al, Neuropathological insights into unexpected cognitive decline in epilepsy, Annals of Neurology (2022). DOI: 10.1002/ana.26557
Journal information:
Annals of Neurology
Source: Read Full Article
