Virtual reality helps unmask impact of moral distress on health-care workers during the pandemic

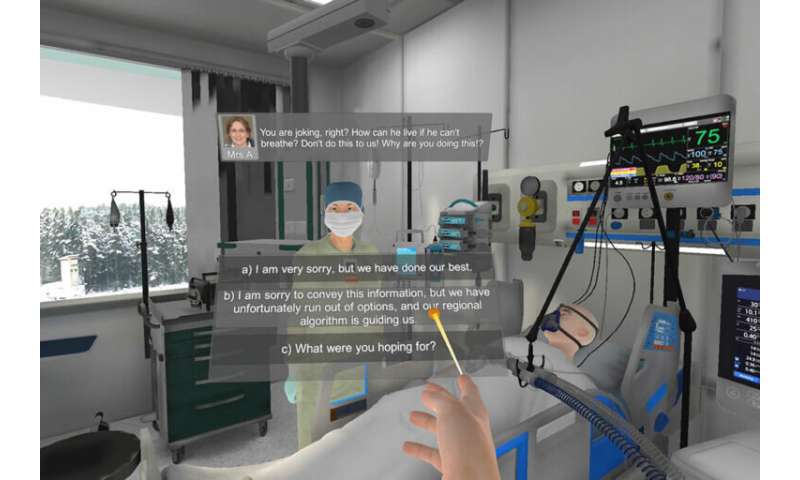
Imagine this: You are a health-care practitioner caring for two patients with severe COVID-19. Both need ventilators. One has a vent but their health is failing rapidly; the other has a chance to survive but there are no ventilators left.
The ventilator is taken from the patient who isn’t doing well and given to the other. You did not influence this decision, but you will need to speak with the families. How does this scenario impact your own moral and mental health?
With the use of virtual reality, a group of researchers from Unity Health Toronto, Ryerson University, Ontario Tech University and the University of Toronto is hoping to understand exactly that.
Led by Dr. Venkat Bhat, a psychiatrist and scientist at St. Michael’s, the team has created a virtual reality simulated scenario where health-care workers who have lived through the pandemic experience what it’s like to provide care with a shortage of ventilators. The team’s goal was to understand whether such a simulation could be created and used by health-care practitioners.
“If you look at digital health interventions for mental health and what has an impact and what does not—there’s very little data out there,” Dr. Bhat said. “Our motivation was to build digital platforms to reduce distress.”
Dr. Elizabeth Peter, a professor at the University of Toronto and researcher in moral distress who worked on this project, describes moral distress as “a result of a constraint where people know what they need to do but the circumstances are such that they cannot do it.” For example, when visitor restrictions limited the amount of time a patient at end-of-life could spend with family, health-care workers may have experienced moral distress.
At one point in the pandemic, the Ontario Critical Care COVID-19 Command Center was prepared for the potential activation of Emergency Standard of Care and the Triage Protocol, designed to help health-care workers determine who receives life-saving care when there are more patients in need of critical care than the number of available ICU beds. The spread of COVID-19 was contained in time and hospitals did not have to enact the protocols.

“People believe, through no fault of their own, that they can’t meet usual standards of care, likely because they don’t have enough resources such as staff or space,” Dr. Peter said. “There are some protective factors, like having support from the team, or being able to have some small power in the organization to make care better that help reduce moral distress.”
Asking health-care practitioners to experience simulated scenarios that trigger moral distress in a safe environment may add to their protective response. Or, as Dr. Bhat suggests, it could showcase to the person and their team that they may need additional support should such scenarios arise.
Study participants echo the moral toll the pandemic, and events from the past year, have had on them.
“If I had gone through this scenario before COVID-19, it would have been different,” says Rebecca Kennedy-Patterson, a nurse in the St. Michael’s TNICU and participant of the study. “This past year has desensitized my approach to these situations. I’m hopeful that this research has impact that’s accessible and can be used by the frontline.”
Dr. Yuliya Rackal, a family physician at St. Michael’s, was also a participant in the study. For her, the scenario reinforced the work she did in the last year to build self-compassion.
“I have small children, online school for them and responsibilities at home and at work—it wasn’t always easy,” she said. “During the pandemic there was nowhere to run from these stresses so I looked at all parts of myself and tried to build self-compassion. I feel like I can better handle hard situations and anxiety because I sat in all these emotions over the course of this year.”
To build a virtual version of scenario that could trigger moral distress, Dr. Bhat recruited experts Dr. Bill Kapralos and Dr. Adam Dubrowski, professors at Ontario Tech University, who specialize in health-care simulation. Their Ph.D. student, Andrei Torres, worked closely with Dr. Bhat’s team and another Ph.D. student, Bill Nguyen, to help code the scenario and create it.
“As we worked on this from December to May, the situation with COVID-19 changed,” Dr. Kapralos said. “Our work was iterative and involved many disciplines to ensure it was realistic.”
Once participants experience the scenario, they are asked to track their emotions on a mental health mobile application that Dr. Bhat co-created with Dr. Sri Krishnan, a professor of engineering at Ryerson University and scientist at iBEST, a joint institute between St. Michael’s and Ryerson that enables collaboration in engineering, science and technology.
“This is a nice example of clinicians and engineers coming together and that is the underlying intention of iBEST,” Dr. Krishnan said. “The problem statement comes from the clinical domain, and engineers can understand the problem.”
Through his previous work with St. Michael’s, Dr. Krishnan had developed relationships with the hospital’s Allan Waters Family Simulation Center, which has been crucial to this work as well. Dr. Doug Campbell, medical director of the center, is a co-principal investigator on this study.
“Our simulation program has been accredited to lead change, guide policy and develop research to answer clinician-based problems and organizational challenges,” Dr. Campbell said. “With this study, we’re trying to address bigger system issues, like how do you prepare people and the system to do things in a moral and ethical way? By helping to understand solutions to protect people from moral distress, we are adding to our work as a driver for good in the organization.”
Now that a dozen health-care workers from across Unity Health have gone through the virtual reality scenario, Dr. Krishnan’s team is helping analyze the data using AI tools. The study has collected active data, in the form of questionnaires and prompts from the mobile application, and passive data over the course of the scenario.
The researchers hope that now they have proven a virtual simulation of moral distress is feasible, the next steps could be to build and measure resilience before people are put in morally distressing situations—whether they be in health-care settings or in other fields such as military work.
Source: Read Full Article
