What you should know about thyroid cancer in adolescents, young adults
Cancer is often thought of as a disease that affects older people, and with the median age of a cancer diagnosis at 66 years, it does. But cancer can be diagnosed at any age.
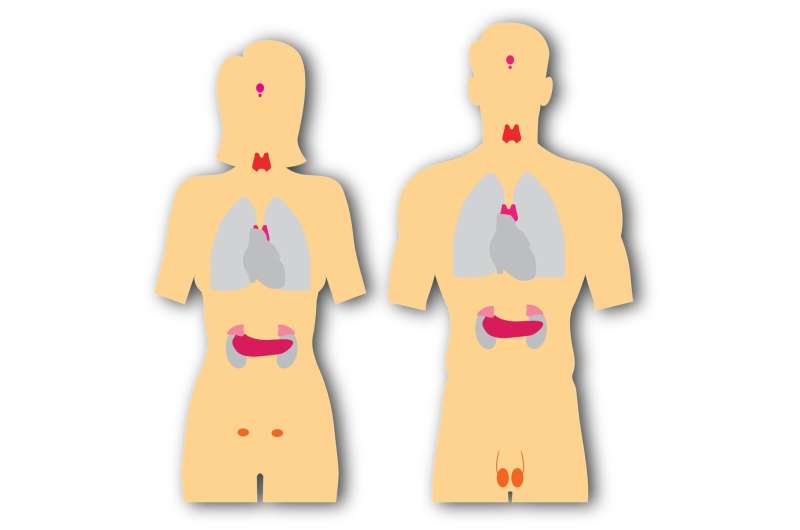
Younger people, including adolescents and young adults between ages 15 and 39—known as AYAs—also are affected by cancer. Thyroid cancer is one of the most common cancers diagnosed in this age group. Fortunately, treatment is straightforward, and when thyroid cancer is treated early, the survival rates are excellent.
Awareness of thyroid cancer, as well as its symptoms and risk factors, can help adolescents and young adults recognize early warning signs and find prompt treatment during a time of life that is often filled with pivotal changes and life events.
Here’s what you should know about thyroid cancer and how it can affect adolescents and young adults:
Should I be concerned about thyroid cancer?
Thyroid cancer has a great prognosis in adolescents and young adults, even though it is often aggressive.
“All cancers are rare in adolescents and young adults, but among those rare cancers, thyroid cancer is the most common in those younger than 30 years of age,” says Siobhan Pittock, M.B., B.Ch., a Mayo Clinic pediatric endocrinologist. And it occurs more often in women.
“When thyroid cancer is diagnosed in younger adults, it may be diagnosed at a more advanced stage,” says M. Regina Castro, M.D., a Mayo Clinic endocrinologist. “We don’t really know why thyroid cancer behaves differently in young adults, but we know that despite the fact that it tends to be more aggressive, the prognosis is still excellent and better than in older adults.”
Many people don’t experience symptoms of thyroid cancer, which can result in the tumor spreading.
“The most common symptom of thyroid cancer is a lump, nodule or a mass toward the back of the neck—sometimes on the side of the neck where the lymph nodes are found,” says Dr. Castro.
However, you may not feel or see the lump. “It is quite common that people don’t notice the lump themselves, and it is found when their doctor feels their neck or it shows up on a scan they are having for other reasons,” says Dr. Pittock.
If you have a family history of thyroid cancer, talk to your health care professional.
The cause of most thyroid cancers is unknown, but high doses of radiation in early childhood for cancer treatment are associated with increased thyroid cancer risk. Genetic factors and family history also are associated with some types of thyroid cancer.
“Medullary thyroid cancer is more genetic. Typically, we see that type of thyroid cancer in patients who develop the condition as part of what we call MEN syndromes, or multiple endocrine neoplasia, where the medullary thyroid cancer is part of an association of other tumors,” says Dr. Castro.
Up to 30% of rare medullary thyroid cancers are associated with genetic syndromes. Having first-degree relatives with thyroid cancer could indicate a genetic mutation in your family, and genetic testing may be recommended.
What should I expect from treatment?
Thyroid cancer treatment is often treated with surgery.
Using surgery as the first-line treatment for thyroid cancer allows your health care professional to remove all or as much of the cancer as possible. It also gives your care team the chance to see if the cancer has spread to nearby lymph nodes, which can happen when cancer is advanced or aggressive.
“Whether the surgery requires a total or partial thyroidectomy will depend on the size of the tumor, findings from imaging, involvement of lymph nodes, and whether or not the contralateral lobe—the side that is not affected—looks entirely normal,” says Dr. Castro.
Thanks to better imaging technology, Dr. Castro says it’s sometimes possible to determine if thyroid cancer is smaller and likely less aggressive. If this is the case, a partial thyroidectomy, also called a lobectomy, might be recommended. She adds that this might be favorable, as it can preserve some of the thyroid’s function.
Radioactive iodine is sometimes used in addition to surgery.
Once your care team determines the stage of your thyroid cancer and its aggressiveness, they might recommend a treatment called radioactive iodine.
Iodine, a mineral found in many foods, is absorbed by the thyroid and used to produce thyroid hormones.
“The most common types of thyroid cancers in adolescents and young adults also absorb iodine. When radioactive iodine is used for the treatment of thyroid cancer, it kills both healthy thyroid and thyroid cancer cells that might be left behind after surgery,” says Dr. Pittock.
In rare cases, you may need additional drug therapy or radiation therapy after surgery.
If your thyroid cancer is too aggressive or it has not been successfully cured by surgery and radioactive iodine, you might need additional treatment, but this isn’t common for adolescents and young adults.
“Chemotherapy is rarely necessary in young adults with thyroid cancer,” says Dr. Castro. “Some patients will need a whole-body scan to determine if they need additional radioactive iodine, but external radiation or chemotherapy is rarely needed.”
Depending on the type of thyroid cancer you have, targeted drug therapies can be effective. These drugs focus on specific characteristics of your thyroid cancer cells that help them thrive.
How will thyroid cancer affect me or my future?
You might have to take hormone medication.
Your thyroid regulates many important functions in your body, including metabolism, body temperature and heart rate. After surgery to remove all or part of your thyroid, your body will no longer be able to do this without help from hormone medication.
“Fortunately, thyroid hormones are safe, effective and inexpensive,” says Dr. Castro. “But for anybody who has had thyroid surgery—and more so if you’ve had a total thyroidectomy—it leaves you with the fact that, for the rest of your life, you’re going to have to take a pill.”
This can be an especially difficult adjustment for young and otherwise healthy people. “At the beginning, it might be tough for somebody who has never needed a medication to have to take a pill every day,” says Dr. Castro.
Family planning might take more preparation.
Because thyroid cancer can occur before or during childbearing years, if you are pregnant or plan on becoming pregnant, you should talk to your health care professional about adjusting your thyroid medication to prepare your body for pregnancy.
“This is an important conversation I have with women who have thyroid conditions,” says Dr. Castro. She adds that while your chances of becoming pregnant won’t necessarily be affected by thyroid medication, your medication dose will need to change during pregnancy, as low thyroid hormone levels could affect your baby’s development.
Thyroid cancer treatments also can affect your family planning timeline. Men who receive radioactive iodine treatment might have decreased sperm counts or infertility for up to two years, according to the American Thyroid Association. While there’s no evidence to suggest that radioactive iodine can cause infertility in women, it’s recommended that women wait six months to one year after treatment before becoming pregnant.
You might need follow-up tests to monitor for recurrence.
Thyroid cancer has a risk of recurrence, but regular monitoring can diagnose new development of thyroid cancer early and help you get treatment as soon as possible.
“The most common type of imaging they will need is an ultrasound,” says Dr. Castro. “Some of the things we look for are: Is there any tumor in the remaining part of the thyroid, is there any evidence of recurrence, and have they developed any abnormal lymph nodes that we need to biopsy or take out?”
Dr. Castro says because thyroid cancers are often more aggressive in adolescents and young adults, they have a higher chance of returning. But this shouldn’t be a cause for alarm.
“Despite all these issues, the vast majority of young adults diagnosed with a thyroid cancer will live a normal lifespan,” says Dr. Castro.
How do I know I am getting the right care?
Find specialized thyroid cancer care.
Thyroid cancer is highly treatable and often curable in adolescents and young adults, but it’s still important to get care from a center that specializes in thyroid cancer and can help you at every stage of your thyroid cancer journey.
At a center that specializes in thyroid cancer, your care team might include experts from oncology, otorhinolaryngology and head and neck surgery, endocrinology, radiation oncology, and pathology. This team approach will provide you the best personalized care during and after treatment.
Centers that specialize in thyroid cancer care also are more likely to offer specialized survivorship care to help you prepare for life after cancer treatment.
“We send all of our patients to our thyroid cancer survivorship clinic, where a provider will meet with them early on and discuss their goals and disease management,” says Dr. Castro.
Find a surgeon who specializes in thyroid cancer surgery.
If your treatment includes surgery, it’s important to find a surgeon who specializes in thyroid cancer surgery. Endocrine or otorhinolaryngologists and head and neck surgeons who specialize in thyroid surgery use the best approaches to give you a good outcome.
But Dr. Castro says patients who need thyroid cancer surgery often don’t receive care from surgeons who specialize in thyroid cancer. “In the United States, the vast majority of thyroid surgeries are done by surgeons who do fewer than 10 of these operations per year.”
This can result in complications.
“Some of the risks of surgery include injury to the nerves that supply the vocal cords. Those nerves travel in close proximity to the thyroid, and if the surgeon doesn’t have the expertise, it can result in injury to the nerve and patients losing their voice or developing hoarseness. In many cases, it can be treated or improved, but in some cases, it’s permanent,” says Dr. Castro.
She adds that it’s not uncommon for parathyroid glands to be injured or accidentally removed at the time of surgery. And this can lead to hypocalcemia or hypoparathyroidism.
“Experienced surgeons are fully aware of these conditions and do their best to avoid these complications. That’s why it’s so important that an expert performs the surgery,” says Dr. Castro.
Dr. Pittock agrees, adds, “It’s OK to ask your surgeon how often they do thyroid cancer surgery and how often their patients have complications.”
Though thyroid cancer has a great prognosis in adolescents and young adults, any cancer diagnosis can be frightening and disrupt your life plans. But great care is available to support you through treatment and recovery and get you back on track.
Source: Read Full Article
