amoxicillin fridge
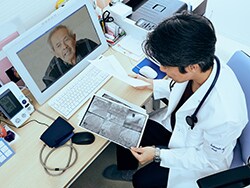
Congress will ultimately approve an extension of Medicare’s telemedicine coverage and the lifting of site restrictions “at least for a few more years,” according to one telemedicine executive.
Peter Antall, MD, chief medical officer of telemedicine company AmWell, made the prediction at a panel discussion at the annual convention of the Health Information Management and Systems Society, in Las Vegas, Nevada.
“If that happens,” he said, “we’re likely to see more trickle-down to commercial payers and, hopefully, where to buy generic nitroglycerin uk without prescription more consistency among state Medicaid agencies with regard to reimbursement, because they tend to follow CMS [Centers for Medicare & Medicaid Services] and Medicare,” said Antall.
However, he added, it will not be easy to get such legislation through Congress. “There is a lot of movement in changing this, but we have a pretty dysfunctional Congress, and it’s been tough to get them to act on this.”
Both the Medicare Payment Advisory Commission (MedPAC) and the Congressional Budget Office (CBO) have expressed reservations about continuing telehealth coverage for Medicare beneficiaries after the public health emergency, noted Ateev Mehrotra, MD, an associate professor at Harvard Medical School, Boston, Massachusetts. He attributed this hesitancy to their expectation that the convenience of telehealth will encourage more people to seek care and thereby raise Medicare spending. Private insurers have similar concerns, he said.
“Payers are thus in a difficult situation: How do you build on the success and advantages of telehealth without breaking the bank? That’s the balancing act,” he said.
Antall agreed but said that CBO should evaluate the available data on cost savings from telehealth. “Most large commercial payers have embraced telehealth and seen cost savings. They wouldn’t be embracing this if they didn’t believe this was a good tool that wouldn’t increase overall costs,” he said.
Mehrotra took issue with Antall’s assertion, saying the health plan executives he has talked to aren’t sure they’ve saved any money through telehealth. Moreover, he said, his research group at Harvard has found evidence that telehealth can increase overall spending.
Virtual Visit Volume Dropping
Although telehealth was vital during the early phase of the COVID-19 pandemic, Mehrotra noted, virtual visit volume is now less than half of what it was then. Currently, it accounts for about 5% to 10% of total healthcare visits. Although this is far higher than the prepandemic level, Mehrotra said, he doesn’t expect that telehealth will ever account for a majority of patient encounters.
Others on the panel agreed that in-person visits will continue to overshadow telehealth. Nevertheless, there was broad agreement that the hybrid system of care delivery that is now emerging, in which the two types of visits are blended, will continue to evolve.
“In the end, we’re not going to use terms like ‘healthcare’ and ‘telehealth,’ ” Antall said. “We’re going to enter a stage where healthcare is much more holistic.”
Margaret Whorisky, an official in charge of Scotland’s telehealth program, noted that the pandemic greatly accelerated the adoption of telehealth in her country. “This all led to a change from telehealth as a ‘nice-to-have’ option to a ‘must-have’ mode of care. It’s now imperative to do it.”
Whorisky added, “We must be mindful of digital exclusion as we use these technologies.”
Two-Tiered System of Telehealth in the US
Mehrotra agreed, noting that in the United States, many people can only have an audio consultation with a practitioner. This has led to a two-tiered system in which the well-off are more likely to have video visits than the poor, who only have their phones. “We don’t want that,” he said. “Many clinical issues can be resolved in a phone call, but video provides a little more information.”
There’s also a significant digital divide between rural and urban areas, he pointed out. Many rural areas lack broadband internet access, and many of their residents don’t have the devices required for video visits.
Although Mehrotra said he was glad that Medicare no longer requires “originating sites” in healthcare settings, people should be allowed to hold telehealth consults in other originating sites, such as cafes or schools, that have internet connections.
Stacy Hurt, a patient consultant who is a survivor of stage IV cancer, concurred with this, noting that with hosting sites, it would be good if patient privacy could be ensured. Patients should be able to get everything they need for a virtual visit, including an interpreter if necessary, she said.
Nationwide Licensing Would Help Patients and Physicians
Hurt said replacing state licenses with nationwide practitioner licenses for telehealth should make things easier for patients. As a patient advocate, she often talks with cancer patients who need a second opinion about their treatment, but they don’t live near a cancer center. “Most people can’t afford to fly around the country to consult a specialist in person,” she said. In her view, specialists should be able to participate in a telehealth consult with a patient anywhere in the country.
The convenience of telehealth also makes it a great option for patients with serious chronic conditions, Hurt observed. “Telehealth should not replace in-person visits, but it can replace visits for things like test results and follow-ups,” she said.
For telehealth to achieve its full potential, Mehrotra said, more attention needs to be paid to the nuts and bolts of the rules governing the technology. For example, he said, state regulations are still highly inconsistent. “There will be reimbursement, but it will be difficult to navigate the labyrinth of state regulations and payment policy,” he said.
In addition, he noted, as the various modes of telehealth — virtual visits, e-consults, portal messaging, and remote monitoring — are reimbursed, patients will have to be educated about how the billing works.
“They need to understand why they’re getting all these different bills, because they have to pay their copayments and deductibles. Communications between patients and providers to help them understand these payments for services that were previously free is going to be a challenge,” he said.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article
