cheap nolvadex montreal

The latest omicron variant BA.5 is fast becoming dominant worldwide, including in New Zealand and Australia. As it continues to surge, reinfection will become increasingly common and this in turn means more people will develop long COVID.
The two most concerning aspects of long COVID are its high prevalence (up to 30% of those infected) and a link between reinfection and a higher risk of harmful outcomes.
American science writer Ed Yong, commenting on government responses to the pandemic, described them as a case of débrouillez-vous, teens get high off flomax which approximates to “you work it out—you’re on your own.”
In the face of official attitudes that are increasingly laissez-faire towards the continuing pandemic, many people no longer take even those precautions over which we have individual control: mask wearing, physical distancing and choosing carefully whether to attend crowded events. The consequences are an increase in both daily case numbers and the lurking burden of long COVID.
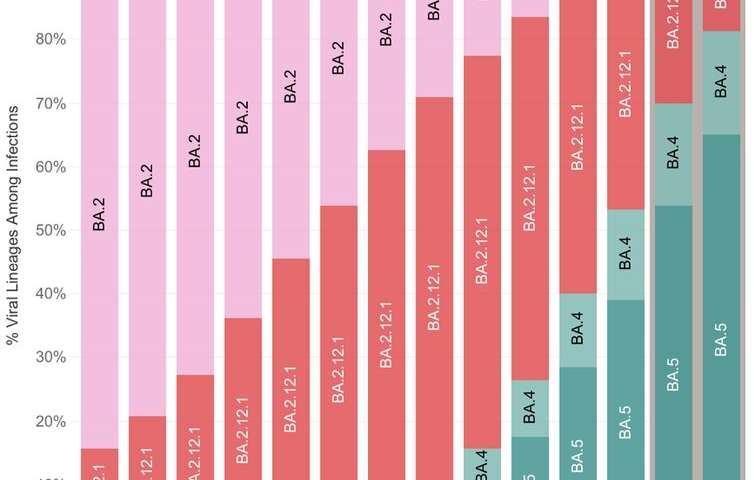
Omicron’s first variant, BA.1, emerged in late 2021, substantially different—clinically and genetically—from earlier variants. It displaced the delta variant and, in early 2022, was itself replaced by BA.2.
The degree to which BA.2 had evolved away from BA.1 is far greater than the genetic distance between the original version of SARS-CoV-2 and the delta variant. BA.5, a sub-variant of BA.2, is now quickly overtaking other variants.
Omicron variants, and BA.5 specifically, show several worrying features. They can evade immunity acquired through earlier infections and breakthrough infections in vaccinated people. BA.5 is better able to infect cells, acting more like delta than the previous omicron variants.
What we know about long COVID
SARS-CoV-2 is not unique in its ability to cause post-acute symptoms and organ damage. Unexplained chronic disability occurred in a minority of patients after Ebola, dengue, polio, the original SARS and West Nile virus infections.
What is different is the sheer size of this pandemic and the number of people affected by long COVID. One of the absolutely critical issues about long COVID is that we should not underestimate it. It is now clear from multiple large studies that:
- It is a set of syndromes
- it affects multiple organs and systems
- it resolves in some but remains persistent in others
- it can be markedly debilitating
- its risk is reduced by vaccination
- its pathology is poorly understood
- we are just beginning to find ways to predict risk and monitor its course
- and management is, at best, ad hoc.
Perhaps most crucially, reinfection may now become a feature of the pandemic for at least the next 12 to 36 months, raising the risk of long COVID with each repeat infection.
Some large studies in Denmark, England, and the U.S. show 20–30% of people who tested positive for COVID-19 experienced at least one post-acute symptom, up to 12 months after infection. Symptoms included loss of smell and taste, fatigue, shortness of breath, reduced limb strength, concentration difficulties, memory disturbance, sleep disturbance and mental or physical exhaustion.
In England, the prevalence of persistent symptoms was higher in women and older people. Obesity, smoking or vaping, hospitalization and deprivation were also associated with a higher probability of persistent symptoms. Those who were hospitalized with COVID in the U.K. showed even more severe outcomes.
In the US, younger survivors were at higher risk than people over 65 for heart-rhythm disturbances and musculo-skeletal pain. This is consistent with other observations that long COVID is not a disorder only of older age.
However, older survivors had a statistically significantly higher risk of developing certain conditions, including kidney failure, clotting disorders, cerebrovascular disease (stroke), type 2 diabetes, muscle disorders and a variety of neurologic and psychiatric conditions.
A US study involving more than five million people shows the risk of long COVID increases with the number of reinfections. But vaccination consistently reduces the risk of long COVID as well as severe disease, hospitalization, ICU and death.
The century-old lesson we’re yet to apply
There are lessons from the 1918–19 influenza pandemic that we need to bring back into our repertoire, not for a month or two but for the long term.
Japan adopted mask wearing as a key public-health element on a short list of available measures. As science writer Laura Spinney notes in her excellent 2017 coverage of the flu pandemic’s history, it “probably marked the beginning of the practice of mask wearing to protect others from one’s own germs.”
In Japan, mask use was compulsory for some, such as the police. In some towns, people were not permitted on public transport or allowed to enter a theater without a mask. Japan had the lowest death rate of all Asian countries in the flu pandemic and is looking to be close to the lowest cumulative mortality in the OECD for the COVID-19 pandemic.
During the 1918–19 pandemic, the U.S., unlike Europe, put considerable effort into public-health interventions, which reduced total mortality. San Francisco, St Louis, Milwaukee and Kansas City had the most effective interventions, reducing transmission rates by 30–50%.
In historian Geoffrey Rice’s Black November and Black Flu (together the most comprehensive coverage of the 1918–19 pandemic in Aotearoa), there are some photographs of people wearing masks and a reference to “gauze masks” for shop keepers. However, there is little evidence to suggest mask wearing was widespread or encouraged in New Zealand.
The influential Italian newspaper Corriere della Sera reported daily death tolls during the 1918–19 flu pandemic until civil authorities asserted it was stirring up anxiety and forced it to stop. As Spinney notes, people could see the exodus of dead bodies from their neighborhoods and the silence was provoking even more anxiety.
The pandemic and the silence conspired to confuse people about the efficacy of public-health measures and compliance dropped off even further. People drifted back to church and race meetings—and left masks at home. Public-health infrastructure collapsed.
Source: Read Full Article
