cialis medicin.dk
The American Thoracic Society now recommends use of average reference equations rather than those based on race or ethnicity for the assessment of pulmonary function in clinical and laboratory practice.
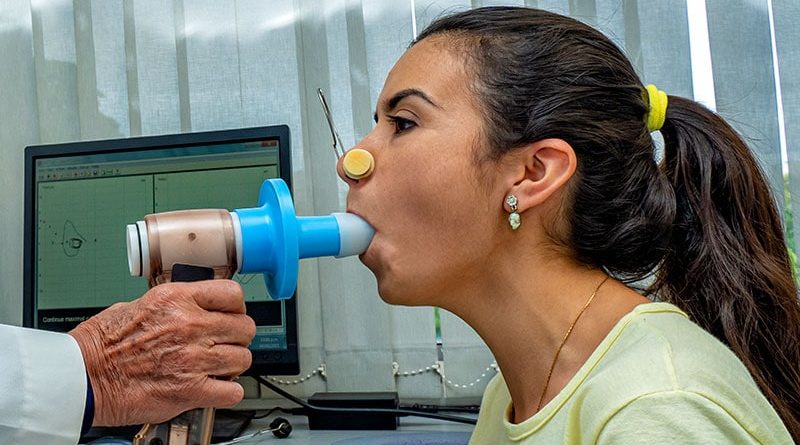
In an official statement to be published in the April 15 issue of the American Journal of Respiratory and Critical Care Medicine, a panel of authors noted that the change was necessary to address concern that use of race and ethnicity in interpretation of spirometry and other pulmonary function tests (PFTs) “contributes to a false view of fixed differences between races and may…contribute to health disparities by norming differences in pulmonary function.”
Concerned that using race as a factor in PFTs in some cases required results from Black patients to be up to 15% lower than those of White patients of similar sex, height, and age for such measurements to be considered abnormal, the ATS in 2021 convened a diverse workshop panel to investigate the issue. The panel did not reach an initial consensus, but several subsequent studies provided strong evidence supporting the elimination of the use of race in PFT reporting and interpretation, according to an ATS release about the official statement.
The new recommendation to use a race-neutral average reference equation from the Global Lung Function Initiative “represents an evolution in thought supported by evidence presented since the most recent technical standards were published,” according to the society.
However, although use of a race-neutral equation is expected to provide more accurate results in many cases, is provigil considered a stimulant the panel stressed the ongoing “uncertainty of comparing an individual’s PFTs with reference values to differentiate health and disease. “They encouraged stakeholders to work to improve interpretation of PFTs, enhance participation of diverse populations in research trials, and address disparities in lung health.
In an accompanying editorial, Kevin C. Wilson, MD, chief of documents and patient education at ATS and a professor in the Department of Medicine at Boston University School of Medicine, noted that although the “recommendation may be controversial” the statement is “an important first step to ignite discussion and accelerate research about race in pulmonary function testing [and] other areas of pulmonary, critical care, and sleep medicine.”
Stressing that “the statement is not intended to be a political statement,” but rather an “evidence-based, scientific expression of a group of experts on a topic important to pulmonary patients,” Wilson wrote that the group employed “the same steps that all official ATS documents must follow” to create the statement.
Barbara P. Yawn, MD, MSc, MSPH, of the University of Minnesota Department of Family and Community Health in Minneapolis, predicted primary care clinicians would be “happy” with the change.

Dr Barbara Yawn
“Race is not a very useful construct in biology or a very useful representation of any individual,” Yawn said. Primary care physicians in the United States now “treat so many people with mixed backgrounds from all different parts of the world, and it can be very difficult for many individuals to even identify their own race and ethnicity.” People may identify differently depending on their social groups, who they live with, and the setting they are in, she said. Beyond this, people doing the testing may inaccurately label a patient’s race and ethnicity.
Yawn also applauded the ATS for calling for ongoing research on PFTs. “It is really, really important that we have more research in this area” to address some of the gaps in evidence, she told Medscape Medical News.
For example, the numbers used in the equations are not based on definitive data, so they are imperfect. “Every time you use [such] an absolute number on an extremely diverse population,” there will be errors, Yawn said.
In addition, she added, in the more than 100 years that spirometry has been used, the technology has changed little. “We need some new tests — something to replace spirometry,” she said.
One potential barrier to implementation of the new race-neutral approach to PFT, Yawn said, is that the neutral equations are not built into most of the spirometers now available. Practitioners both in primary care and other settings will need to learn how to calibrate the equipment for the new equations.
Use of spirometry in primary care settings has become more complicated in the COVID-19 era. Yawn noted that early in the pandemic many health systems stopped spirometry testing because of concerns about spreading the virus.
“Unfortunately, they have not put them back in place, making spirometry more difficult to obtain in the primary care setting,” she said. And since patients often skip care if it requires referrals or additional visits, this testing may go undone or be postponed, which could result in delayed treatment for lung conditions.
Yawn reports no relevant financial relationships.
Am J Respir Crit Care Med. Published in the April 15 issue. Full text, Editorial
Sarah Tilyou is a medical journalist in New York.
Source: Read Full Article