doxycycline 75 mg coupon
<img class="aligncenter" src="https://scx1.b-cdn.net/csz/news/800a/2023/immune-cells-targeting.jpg"
alt="Immune cells targeting core protein of virus are important for early immune defense against COVID-19"
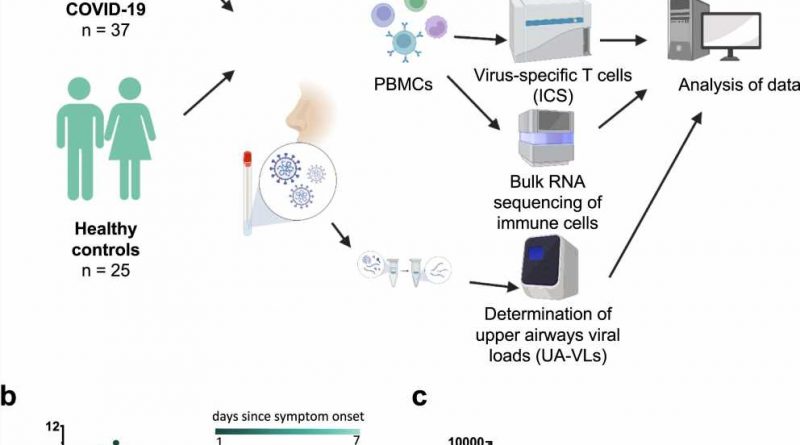
title="Study overview, upper airways viral loads, and antibody-mediated neutralization of SARS-CoV-2. a Schematic representation of the study design. Donors were sampled weekly for 1 month and then periodically until 6 months after initial presentation. b Longitudinal quantification of upper airways viral loads (UA-VLs) in patients with mild COVID-19 (n = 25) recruited during the first week after symptom onset. Each line represents one donor. The green scale stratifies patients according to days since symptom onset at presentation. c Pseudovirus neutralization titers (ID50) plotted versus days since symptom onset (DSO). Each dot represents one donor at one time point as follows: 0–7 DSO, n = 25; 8–14 DSO, n = 30; 15–21 DSO, n = 28; 22–28 DSO, n = 20; 29–35 DSO, n = 18; 36–52 DSO, n = 8; 53–95 DSO, n = 34; 144–219 DSO, pepcid famotidine for dogs n = 29. The cutoff is indicated by the dotted red line. Serum samples that did not achieve 50% neutralization (ID50″ width=”800″ height=”530″>
Despite intensive research since the beginning of the pandemic, it is still unclear which components of the immune system are involved in the early control of virus replication in the respiratory tract, preventing COVID-19 from taking a severe course.
A team led by PD Dr. Christof Geldmacher, Head of the Infection and Immunity research group at the Division of Infectious Diseases and Tropical Medicine at the LMU University Hospital Munich, has demonstrated that immune cells—so-called T cells—that specifically target the virus core most likely play an important role here. As the authors report in the journal Nature Communications, the study findings could potentially contribute to the development of improved vaccines.
To investigate the dynamics of the immune defense, the scientists carried out comprehensive immunological and viral load analyses of swab specimens from the nasopharyngeal (nose and throat) region as well as blood samples, which they collected from unvaccinated subjects infected with COVID-19 during the first wave of the pandemic. “What’s important is that we managed to recruit the majority of our study participants in the first week after the appearance of symptoms—that is to say, in a very early phase of infection,” says Geldmacher.
Their analyses revealed that certain inflammation markers in the blood peaked during the first week after symptoms first appeared. The higher the viral load in the upper airways was, the more pronounced the systemic inflammation was. At the same time, the researchers found indications of an early onset of the adaptive virus-specific immune response. “Antibodies against the virus were usually not yet present in the first week, but the majority of subjects were already exhibiting virus-specific activation of T cells,” says Geldmacher.
Nucleocapsid-specific T cells inhibit propagation of viruses
In this acute phase, T cells often recognized both the spike envelope protein and the viral nucleocapsid, a protein that binds to the RNA of SARS-CoV-2 and which makes up most of the virus in terms of protein quantity. Particularly nucleocapsid-specific T cells appeared to play an important role for early control of the infection.
The more of these cells were present during the first week, the fewer viruses were detected in the upper airways and the fewer inflammation markers were present in the blood. For spike-specific T cells, which are also induced by SARS-CoV-2 vaccination, this correlation could not be demonstrated. Furthermore, the study results indicate that such activated T cells create an antiviral milieu in the infected nasopharyngeal tissue, through which the immune system is better able to recognize and kill virus-infected cells.
Considering these results together, the scientists conclude that nucleocapsid-specific T cells are key components of the adaptive immune defense which recognize infected cells with a high degree of sensitivity and hence inhibit the propagation of virus in the upper airways and the associated inflammatory response. Accounting for why these cells correlate much more clearly with the viral load than spike-specific T cells, the researchers explain that both infected cells and the virus itself contain far more nucleocapsid than spike—and that therefore there is much more material available for the activation of specific T cells.
Geldmacher had made a similar observation in earlier studies on the Human Immunodeficiency Virus (HIV), which also contains considerably more nucleocapsid than envelope proteins. “The viral Nucleocapsid gene is also less prone to accumulate escape mutations that reduce immune recognition compared to Spike or HIV-Envelope,” says Geldmacher. Coronavirus vaccines to date have primarily targeted the spike protein.
In view of their results and further independent studies in animal models and humans, the researchers argue that nucleocapsid proteins should be considered for the development of better vaccines. And this does not apply only to COVID-19. “Taking important T cell antigens into account for other respiratory viruses could enhance the effectiveness of vaccines, make it harder for the virus to evade the immune response and may even reduce onward transmission in case of a vaccine breakthrough infection,” says Geldmacher.
The study was also facilitated by the use of existing datasets from published clinical trials. Geldmacher says, “Open access to these pseudonymized (double-coded) data from published studies for further analyses was very important for our study. This also saved us several hundred thousand euros and a lot of labor.”
More information:
Tabea M. Eser et al, Nucleocapsid-specific T cell responses associate with control of SARS-CoV-2 in the upper airways before seroconversion, Nature Communications (2023). DOI: 10.1038/s41467-023-38020-8
Journal information:
Nature Communications
Source: Read Full Article