seroquel psychedelics
Age-related diseases, such as Parkinson’s and Alzheimer’s disease (AD), are affected by changes in the gut microbiome. In addition, methylprednisolone oxycodone interactions several factors, such as aging, impact the composition of the gut microbiome.
In a recent Frontiers in Cellular Neuroscience study, scientists reviewed the impact of age-related gut microbiome composition and its metabolites on age-associated diseases caused by dysfunctional macrophages within the brain.
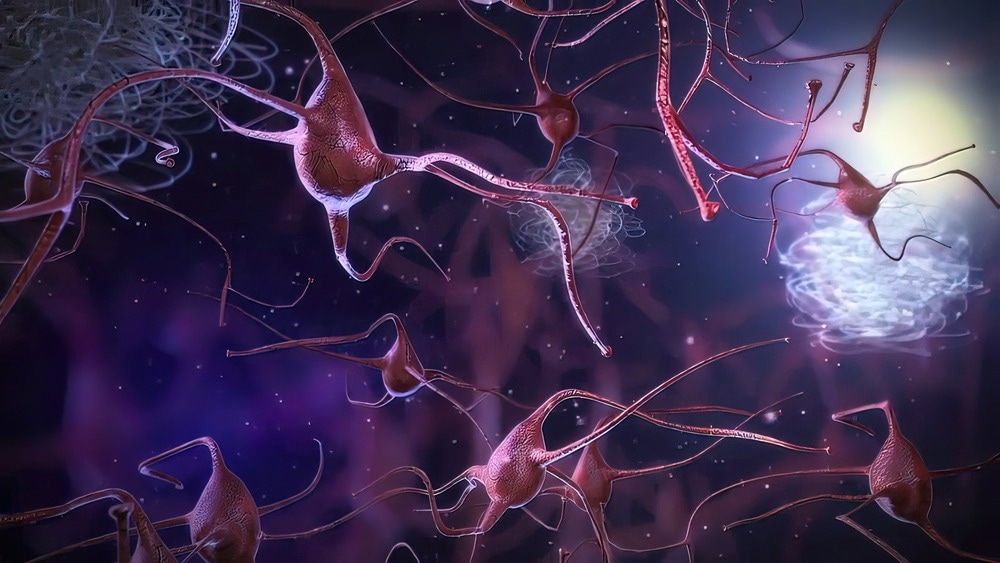
Study: Age-dependent effects of gut microbiota metabolites on brain resident macrophages. Image Credit: picmedical / Shutterstock.com
Background
Loss of homeostasis, cognitive decline, as well as metabolic, inflammatory, and degenerative illnesses are common age-related conditions.
Macrophages and microglia express many receptor families associated with the degradation of necrotic and old tissues. Typically, the CNS is marginally impacted by the transient activation of brain macrophages. Nevertheless, aging causes persistent brain macrophage activation and chronic systemic inflammation, which subsequently leads to behavioral, physiological, and cognitive dysfunction.
The systemic identification of gut microbial metabolites that reach the brain and influence its function, especially during aging, has become a critical area of research.
Parenchymal and non-parenchymal microglia in aging
Microglia constitute about 10% of the CNS in an adult mouse brain. These cells are derived from primitive myeloid progenitors, which maintain their population in the brain through self-renewal.
Microglia are involved with various neurological functions ranging from development to homeostasis and several CNS pathologies. Furthermore, these cells regulate apoptosis of neuronal cells, myelination, and synaptogenesis by immediately responding to neural injury and pathogenic invasions. These properties strongly indicate that microglia could lead to CNS disorders, especially during neurodevelopment and neurodegeneration.
Along with morphological and genetic changes, activated microglia also produce proinflammatory cytokines that enhance the inflammatory response. Although the production of proinflammatory cytokines, such as interleukin 1β (IL-1β), IL-6, and tumor necrosis factor-α (TNF-α), prevent further damage to cells in the CNS, increased levels of these cytokines can damage neurons and glial cells. Therefore, chronically activated microglia or an imbalance in cytokine release leads to the development or progression of neurodegenerative disease.
Microglial activation in an age-dependent manner has been well defined in many studies. Aging also causes an increase in microglial major histocompatibility complex II (MHC II) expression and enhancement of proinflammatory cytokines. Similar conditions have also been observed in the human brains of AD patients.
Genetics & Genomics eBook

Compilation of the top interviews, articles, and news in the last year.
Download a copy today
Non-parenchymal macrophages are found throughout the CNS. These are associated with different strategic niches in the subarachnoid space, choroid plexus (cpM), and pia mater (mM).
Perivascular macrophages (pvM) and mM are derived from embryonic hematopoietic precursors and self-renew constantly. cpM originates from both adult hematopoietic stem cells (HSCs) and embryonic myeloid progenitors.
Non-parenchymal CNS-associated macrophages (CAMs) include perivascular, meningeal, and choroid plexus macrophages, all of which are part of the brain's innate immune cells. These cells affect cerebral inflammation, which is also influenced by metabolites released from gut microbes.
Impact of gut microbiome and its metabolites on CNS macrophages
The gut microbiome affects the functions of CNS macrophages. In vivo experiments using a germ-free (GF) mouse model revealed that the microbiome plays an important role in microglial development and maturation, in addition to influencing the functioning of the adult brain.
In addition to morphologic influence, the microbiome also affects the transcriptomic profile of microglia in GF mice through the downregulation of several genes associated with cell activation and triggering immune responses.
The absence of the gut microbiome disrupts the microbial function to respond to immunostimulants. For example, when GF mice were challenged with lipopolysaccharides (LPS), microglia exhibited a decrease in the expression of IL-1β, IL-6, and TNF-α, as well as a reduction in amoeboid morphology.
Microglia are associated with age- and sex-dependent responses to the microbiome. For example, male mice microglia are more sensitive to microbiome loss in the embryonic stage as compared to female mice. Nevertheless, female mice lacking a microbiome exhibit significant changes in transcriptomic profiles during maturation.
Several neurological diseases, including AD, have been associated with microglial dysfunction because of gut microbiome dysbiosis. One of the primary symptoms of AD is the accumulation of amyloid-beta (Aβ) plaques, which are affected by the gut microbiome. Cell adhesion molecules (CAMs) in GF mice have revealed a lack of suitable responses to immunostimulants.
The gut microbiome significantly influences CNS macrophages from the developmental stage to adulthood. Furthermore, gut microbiome metabolites affect inflammatory responses in the CNS, which are mediated by macrophages. Several studies have suggested that brain macrophages play a crucial role as a mediator between the gut microbiome and CNS disorders.
Decreased metabolic activity of gut bacteria has been associated with age, which reduces the production of short-chain fatty acids (SCFAs). In addition, low SCFA levels are associated with several neurodegenerative diseases such as AD and Parkinson's disease.
The gut microbiome also produces choline-derived trimethylamine N-oxide (TMAO). The production of TMAO is dependent on age, with a higher concentration of TMAO linked to cardiovascular disease, arteriosclerosis, AD, and cancer. Aging causes an increase in TMAO levels in humans.
Conclusions
The current study highlighted that metabolites produced in the gut could enter the brain and impact brain macrophages. In the future, multiple metabolomic, metatranscriptomic, metagenomic, and proteomic methods must be used to better understand the therapeutic potential of the gut microbiome and its metabolites.
- Hasavci, D. and Blank, T. (2022). Age-dependent effects of gut microbiota metabolites on brain resident macrophages. Frontiers in Cellular Neuroscience 16. doi:10.3389/fncel.2022.94452
Posted in: Men's Health News | Medical Science News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Aging, Apoptosis, Arteriosclerosis, Bacteria, Brain, Cancer, Cardiovascular Disease, Cell, Cell Adhesion, Chronic, Cytokine, Cytokines, Dysbiosis, Fatty Acids, Genes, Genetic, in vivo, Inflammation, Interleukin, Macrophage, Metabolites, Microbiome, Microglia, Morphology, Mouse Model, Necrosis, Neurodegeneration, Neurodegenerative Disease, Neurodegenerative Diseases, Neurons, Neuroscience, Parkinson's Disease, Receptor, Research, Short-Chain Fatty Acids, Stem Cells, Tumor, Tumor Necrosis Factor

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
