Contraception and STIs
The term contraception refers to any method which prevents pregnancy. Different methods are used, some of which are hormonal and others non-hormonal. Some methods also help the user to avoid acquiring sexually transmitted infections.
A sexually transmitted infection (STI) is one which is carried to other people via sexual activities. It may be caused by bacteria, viruses, or parasites. The most common STI is caused by the human papilloma virus (HPV), but other common examples include gonorrhea, chlamydia, HIV, syphilis, HPV, herpes genitalis, and louse infestation.
Modes of sexual transmission include vaginal intercourse, oral, anal, or any combination of these. Safe sexual practices help to avoid acquiring STIs, by averting unprotected intercourse or any sexual activity with a partner who has such an infection already or is at high risk of one.
Contraceptives which reduce STI risk
1. Condoms
Most people use contraception to prevent pregnancy, but safe sex is equally important to avoid STIs if the partners are not in a monogamous relationship. The only proven contraceptive method to reduce the risk of STI transmission is the male condom. Latex is the best material, but polyurethane is effective in the case of latex allergy.

It is important to know that natural condoms, or ones made of lambskin, are not effective as the tiny pores in the leather allow viruses to pass through. A condom is not 100 percent protective as transmission may occur through the areas not covered by the condom. Moreover, it has to be used for each instance of sexual intercourse to be effective.
The condom has become more popular since the beginning of the modern epidemic of HIV infection, but has been around for thousands of years prior to this.
The female condom is similar in its composition to the male condom, but its effectiveness in blocking the spread of viruses has not been equally studied. It is designed to allow the female partner to control contraception during intercourse, and its fitting makes it impossible for accidental impregnation to occur, unlike the use of male condoms, because when it breaks it slips out of the vagina and not into it.
The use of a condom with every sexual act reduces the risk of several STIs, including gonorrhea, chlamydia, herpes and other ulcerating viruses, bacterial vaginosis, and pelvic inflammatory disease.
2. Dams
The dental dam is a thin piece of latex which is spread over the perineum and vulva, to prevent direct skin-skin or mucosal contact between the partners during oral sex. It is used along with male or female condoms.
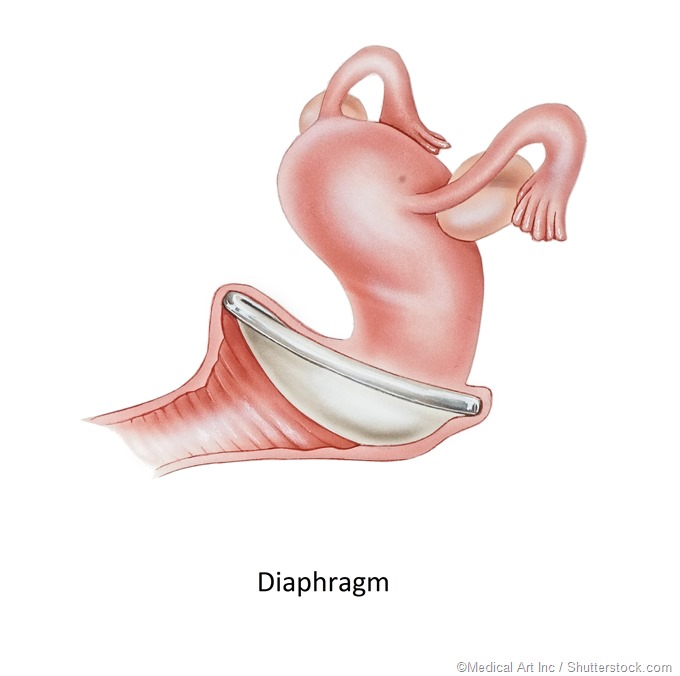
3. Diaphragms and caps
Vaginal diaphragms and cervical caps reduce STI transmission in the upper part of the reproductive tract but not through the perineum or the lower vagina.
Diaphragms and cervical caps prevent cervical and upper genital tract infection but not vaginal and external genital infection.
Risk factors for STI
The following factors increase the chances of STI:
- Increased number of partners
- Having a partner who engages in sexual activity with more than one partner
- Regular use of combined oral contraceptives, which increases the risk of chlamydial infection of the lower reproductive and genital tract
- Insertion of IUDs for women who have pre-existing infections of the pelvic organs, who are sexually promiscuous, or who have non-monogamous partners
- The contraceptive sponge contains the spermicide nonoxynol-9, which inactivates sperms. It also absorbs semen, and acts as a mechanical barrier to the cervix. It is interesting to note that this spermicide has been reported to increase the risk of STI transmission, possibly by generating ulceration of the genital mucosa due to its detergent properties
- Oral contraceptives have been associated with an almost doubled risk of vaginal candidiasis and genital chlamydial infection, but a lower risk of bacterial vaginosis, when compared to no contraception
- The long-acting progestin injectable depot medroxyprogesterone acetate (DMPA) is associated with a lower risk of several STIs, including trichomoniasis, bacterial vaginosis, and pelvic inflammatory disease. The risk of chlamydial infection is significantly increased, however
Dual protection
Because of the importance of preventing both unintended pregnancy and STI transmission, the use of a barrier method with another effective method of contraception is recommended. This is because the efficacy of a condom is not as high as that of other methods in preventing pregnancy. However, the technique of proper condom use should be mastered, as condom breakage is just as disastrous when it comes to STIs as it is in allowing pregnancy to occur. The second method may be a long-acting form of contraception. Even sterilized women need to use dual contraception if they have sex with infected partners or with multiple partners.
The general need to protect oneself against STIs is emphasized by considering the vulnerability, otherwise, to the acquisition of chronic and serious STIs such as HIV. The use of hormonal contraception should be supplemented by sexual fidelity, or by the use of condoms for every sexual act if repeated with multiple partners.
References
- http://services.unimelb.edu.au/health/sexual/contraception
- https://www.nichd.nih.gov/health/topics/contraception/conditioninfo/Pages/std-prevention.aspx
- https://www.ncbi.nlm.nih.gov/pubmed/12318983
- https://www.betterhealth.vic.gov.au/health/healthyliving/contraception-choices
- https://www.healthdirect.gov.au/contraception-options
- https://www.womenshealth.gov/a-z-topics/birth-control-methods
- https://www.ncbi.nlm.nih.gov/pubmed/11518896
Further Reading
- All Contraception Content
- Advantages and Disadvantages of the Contraceptive Patch
- Advantages and Disadvantages of the Contraceptive Implant
- Advantages and Disadvantages of the Contraceptive Vaginal Ring
- Do Contraceptive Injections Affect Bones?
Last Updated: Feb 26, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
