Trichinellosis Diagnosis
Trichinellosis represents a food-borne zoonotic parasitic disease caused by roundworms from the genus Trichinella.
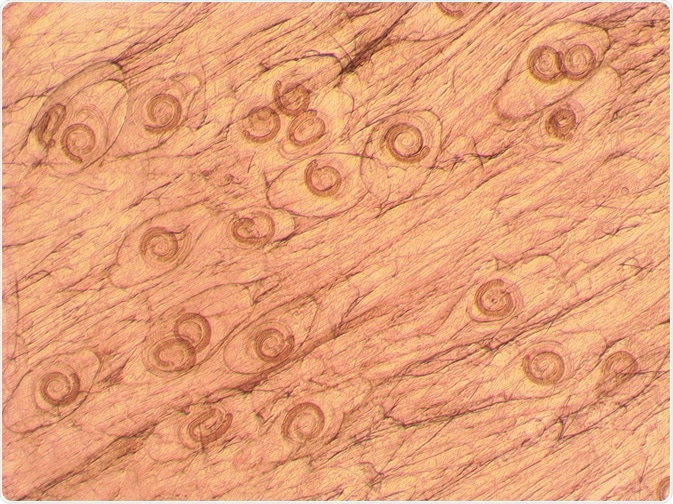 Trichinella spiralis. Credit: olgaru 79/ Shutterstock.com
Trichinella spiralis. Credit: olgaru 79/ Shutterstock.com
It is somewhat difficult to make an early clinical diagnosis of this condition because there are few pathognomonic signs or symptoms. There are problems in diagnosing later chronic forms as well, further complicated by difficulties in the differential diagnosis of trichinellosis when confronted with an atypical clinical course or with an isolated case.
Hence, the diagnosis of Trichinella infection should be centered on three principal criteria: clinical findings (identification of characteristic signs and symptoms), laboratory findings (non-specific laboratory parameters, detection of larvae in muscles and/or antibody detection), as well as epidemiological investigation (recognition of the infectious source and origin).
Laboratory findings
In virtually every case of clinically manifest trichinellosis, an increased number of leukocytes is observed accompanied by an increased number of eosinophils, though this is a relatively non-specific laboratory sign. This is also known as eosinophilia, and it tends to appear before the development of overt signs and symptoms, usually between the second and the fourth week of the infection.
Moreover, an elevated level of muscle enzymes (most notably creatinine phosphokinase, aldolase and/or lactate dehydrogenase) can be seen in blood as an indication of myositis (i.e. muscle invasion). This is concurrently observed in up to 90% of infected individuals with eosinophilia, and may last for up to four months.
Direct parasitological diagnosis
If patients are suspected to have trichinellosis, the direct identification of parasites necessitates a muscle biopsy. In humans, the deltoid muscle is a preferred biopsy site as it is quite accessible. Trichinella larvae may be discovered in the muscle biopsy by trichinoscopy, artificial digestion with hydrochloric acid and the enzyme pepsin, or by histological analysis.
However, the risk of potential complications because of the invasive nature of muscle biopsy is an impediment to the direct demonstration of Trichinella parasites in humans. The technique is also expensive and quite painful, which is the reason why other procedures to diagnose the condition are used instead.
Serologic diagnosis
The detection of specific anti-Trichinella antibodies in human serum is vital for the diagnosis. Their detection in humans after primary infection depends chiefly on the seroconversion interval. An early upsurge in the IgE class of antibodies (which is observed in most cases) suggests that the immune system responds to Trichinella infection by an allergic reaction in the form of edema or a cutaneous rash.
The demonstration of IgG antibodies is taken as a proof of infection. These may be detected from 12 to 60 days following primary infection, depending on the parasite species involved, the immune response and the larval infective dose.
Enzyme-linked immunosorbent assay (ELISA) still represents the most commonly employed diagnostic technique, although the indirect fluorescent antibody test is sometimes used as well. The latex agglutination test is used when rapid diagnosis is required.
Immunoblotting is considered a confirmatory test, since it may confirm positive cases or exclude false-positive serological test results. Western blotting is therefore a useful tool for ruling out potential cross-reactions with other parasites on ELISA and indirect fluorescent antibody testing. Due to its cost and labor-intensiveness, it is not used as a screening test.
Epidemiologic investigation
While serologic testing, such as those mentioned previously, may be useful in epidemiologic investigations and surveillance of outbreaks in domestic animals and wildlife, diagnostic testing is shifting to the use of rapid molecular methods that can identify a single larva to the level of species or even genotype.
Swift and accurate identification of the source of infection that can be traced back to the farm of origin is a very important step to gain a precise count of the maximum number of individuals who might have been introduced to contaminated food. By definition, an outbreak of trichinellosis requires at least one laboratory-confirmed case.
Sources
- http://cmr.asm.org/content/22/1/127.full
- https://www.ncbi.nlm.nih.gov/pubmed/15482143
- https://www.cdc.gov/parasites/trichinellosis/
- http://www.tandfonline.com/doi/abs/10.1517/14656566.3.8.1117
- vphcap.vet.cmu.ac.th/…/Chapter2.pdf
- Pozio E. Foodborne nematodes. In: Gajadhar AA, editor. Foodborne Parasites in the Food Supply Web: Occurrence and Control. Woodhead Publishing (Elsevier), 2015; pp. 165-200.
Further Reading
- All Roundworm Content
- Roundworm Transmission from Pets to Humans
- What is Visceral Larva Migrans?
- All Trichinellosis Content
- Trichinellosis Epidemiology
Last Updated: May 27, 2019

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article
