Examining the determinants of persistent and severe COVID-19
As COVID-19 wreaks havoc across the globe, one characteristic of the infection has not gone unnoticed. The disease is heterogeneous in nature with symptoms and severity of the condition spanning a wide range. The medical community now believes this is attributed to variations in the human hosts’ biology and has little to do with the virus per se.
Shedding some light on this conundrum are Associate Professor SUMI Tomonari from Okayama University, Research Institute for Interdisciplinary Science (RIIS) and Associate Professor Kouji Harada from Toyohashi University of Technology, the Center for IT-based Education (CITE). The duo recently reported their findings on imbalances in the host immune system that facilitate persistent or severe forms of the disease in some patients.
The researchers commenced their study by computer simulations with models based on a host’s immune system and its natural response to SARS-CoV-2 exposure. Mathematical equations for the dynamics of cells infected by SARS-CoV-2 were plugged in to predict their behavior.
The immune system has messenger cells known as dendritic cells (DCs). These cells report information (in the form of antigens) about the invaders to the warriors, or T cells, of the immune system. The model showed that at the onset of infection, DCs from infected tissues were activated and then antibodies to neutralize SARS-CoV-2 gradually started building.
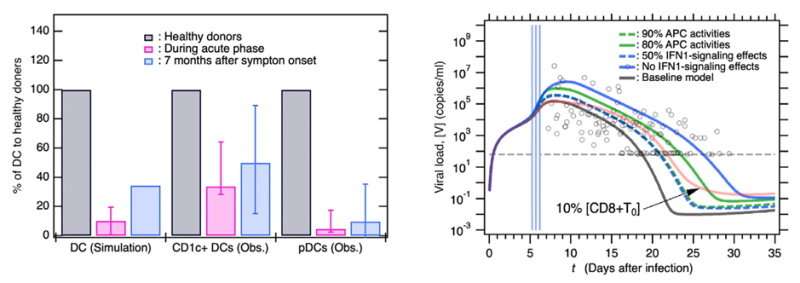
To investigate long-term COVID-19, the behavior of DCs 7 months after infection was evaluated by the computer simulation. The baseline model simulation revealed that DCs drastically decreased during the peak of infection and slowly built up again. However, they tended to remain below pre-infection levels. These observations were similar to those seen in clinical patient samples. It seemed like low DC levels were associated with tenacious long-term infection.
The subsequent step was to understand if DC function contributed to disease severity. It was found that a deficiency of the antigen-reporting function of DCs and lowered levels of chemicals known as interferons released by them were related to severe symptoms. A decrease in both these functions resulted in higher amounts of virus in the blood (viral load).
What’s more, the researchers also found two factors that affected the virus’s ability to replicate in the host, namely, antigen-reporting DCs and the presence of antibodies against the virus. Anomalies in these functions could hamper viral clearance, enabling it to stay in the body longer than expected, whereas a high ability of these immune functions suppresses viral replication and yields prompt viral clearance.
Components of immune signaling that directly affect the outcome of COVID-19 infection were revealed in this study. ” Our mathematical model predicted the persistent DC reduction and showed that certain patients with severe and even mild symptoms could not effectively eliminate the virus and could potentially develop long COVID,” concludes the duo. A better understanding of these immune responses could help shape the prognosis of and therapeutic interventions against COVID-19.
Source: Read Full Article
