Plant-based diets shown to lower blood pressure even with limited meat and dairy
Consuming a plant-based diet can lower blood pressure even if small amounts of meat and dairy are consumed too, according to new research from the University of Warwick.
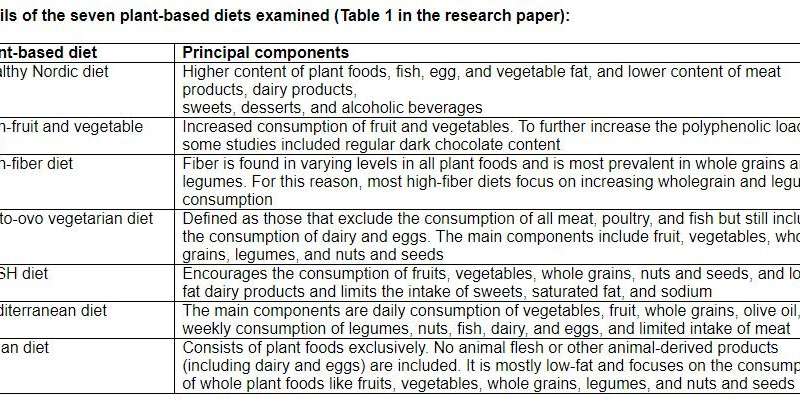
Published online by a team from Warwick Medical School in the Journal of Hypertension today (25 July), they argue that any effort to increase plant-based foods in your diet and limit animal products is likely to benefit your blood pressure and reduce your risk of heart attacks, strokes and cardiovascular disease. They conducted a systematic review of previous research from controlled clinical trials to compare seven plant-based diets, several of which included animal products in small amounts, to a standardised control diet and the impact that these had on individuals’ blood pressure.
Plant-based diets support high consumption of fruits, vegetables, whole grains, legumes, nuts and seeds, limiting the consumption of most or all animal products (mainly meat and diary). (See Notes to Editors for further details)
High blood pressure is the leading risk factor globally for heart attacks, strokes and other cardiovascular diseases. A reduction in blood pressure has important health benefits both for individuals and for populations. Unhealthy diets are responsible for more deaths and disabilities globally than tobacco use, high alcohol intake, drug use and unsafe sex put together. An increased consumption of whole grains, vegetables, nuts and seeds, and fruit, as achieved in plant-based diets, could avert up to 1.7, 1.8, 2.5 and 4.9 million deaths globally respectively every year according to previous research.
Vegetarian and vegan diets with complete absence of animal products are already known to lower blood pressure compared to omnivorous diets. Their feasibility and sustainability are, however, limited. Until now, it has not been known whether a complete absence of animal products is necessary in plant-based dietary patterns to achieve a significant beneficial effect on blood pressure.
Lead author Joshua Gibbs, a student in the University of Warwick School of Life Sciences, said: “We reviewed 41 studies involving 8,416 participants, in which the effects of seven different plant-based diets (including DASH, Mediterranean, Vegetarian, Vegan, Nordic, high fibre and high fruit and vegetables) on blood pressure were studied in controlled clinical trials. A systematic review and meta-analysis of these studies showed that most of these diets lowered blood pressure. The DASH diet had the largest effect reducing blood pressure by 5.53/3.79 mmHg compared to a control diet, and by 8.74/6.05 mmHg when compared to a ‘usual’ diet.
“A blood pressure reduction of the scale caused by a higher consumption of plant-based diets, even with limited animal products would result in a 14% reduction in strokes, a 9% reduction in heart attacks and a 7% reduction in overall mortality.
“This is a significant finding as it highlights that complete eradication of animal products is not necessary to produce reductions and improvements in blood pressure. Essentially, any shift towards a plant-based diet is a good one.”
Senior author Professor Francesco Cappuccio of Warwick Medical School said: “The adoption of plant-based dietary patterns would also play a role in global food sustainability and security. They would contribute to a reduction in land use due to human activities, to global water conservation and to a significant reduction in global greenhouse gas emission.
“The study shows the efficacy of a plant-based diet on blood pressure. However, the translation of this knowledge into real benefits to people, i.e. its effectiveness, depends on a variety of factors related to both individual choices and to governments’ policy decisions. For example, for an individual, the ability to adopt a plant-based diet would be influenced by socio-economic factors (costs, availability, access), perceived benefits and difficulties, resistance to change, age, health status, low adherence due to palatability and acceptance.
Source: Read Full Article
