Team develops an approach to facilitate the diagnosis of tuberculosis as cause of death
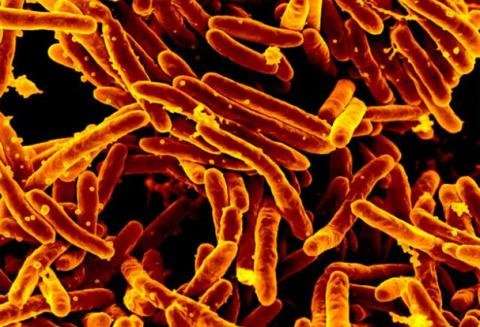
The molecular test ‘Xpert Ultra’ combined with a minimally invasive autopsy technique can facilitate the diagnosis of tuberculosis as cause of death in low-income countries, according to a study led by the Barcelona Institute for Global Health (ISGlobal), an institution supported by the “la Caixa” Foundation. This technology, which can be applied to easily available bodily fluids such as plasma, could be a valuable tool in regions where the disease burden is high.
Tuberculosis (TB) is estimated to have caused one 1.5 million deaths in 2018. However, the real number of deaths caused by the disease remains unknown: around 30% of cases are not diagnosed or not reported and, even if they are reported, it is not easy to determine whether it was the cause of death.
The complete autopsy is the gold standard for establishing the cause of death, but the procedure is rarely performed in low-income countries, due to a shortage of trained pathologists and low acceptability by relatives. For this reason, an ISGlobal team has worked over the last years to develop and validate the minimally invasive autopsy (MIA) technique. “This technique is easier and faster to perform in low-income countries and better accepted by the relatives, since it takes samples from different organs with fine biopsy needles that barely leave a mark,” explains Jaume Ordi, co-coordinator of the CADMIA and CADMIA plus projects, funded by the Bill & Melinda Gates Foundation and of which these findings form part.
The present study led by Miguel Martínez, ISGlobal researcher and microbiologist at the Hospital Clinic, evaluated the accuracy of a rapid and simple molecular test, called Xpert MTB/RIF Ultra, for diagnosing tuberculosis as the cause of death in patients who died in the Central Hospital of Maputo, in Mozambique. To do so, the research team used samples obtained by MIA from the lung, central nervous system, cerebrospinal fluid, and plasma of 117 patients with or without TB diagnosis at the time of death.
A high predictive value
Xpert Ultra applied to MIA lung samples correctly detected 78% of death by TB cases, and 67% when using plasma samples. “The combined analysis of lung and central nervous system would only have missed 15% of TB deaths,” says Alberto García-Basteiro, first author of the study. In a region such as Mozambique, where mortality by TB and HIV is very high, positivity in plasma MIA samples had a high predictive value (>90%) for establishing TB as cause of death.
Source: Read Full Article
