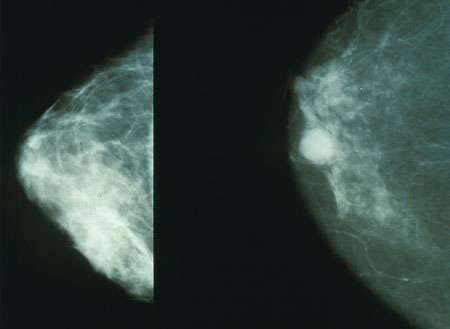
Trial finds benefit of immunotherapy-chemotherapy combination in early-stage triple-negative breast cancer
Adding an immunotherapy agent to a three-drug chemotherapy regimen can improve the likelihood that early-stage triple-negative breast cancer will recede to undetectable levels, data from a clinical trial led by Dana-Farber/Brigham and Women’s Cancer Center suggests.
The results of the trial, dubbed the IMpassion031 study, will be presented at the 2020 Congress of the European Society for Medical Oncology (ESMO), being held virtually Sept. 19-21.
The Phase III trial, which enrolled 333 people with previously untreated triple-negative breast cancer, evaluated the safety and effectiveness of atezolizumab—an immune checkpoint inhibitor which exposes cancer to an immune system attack by blocking the PD-L1 protein on tumor cells—in conjunction with a standard chemotherapy combination. The findings are part of a growing body of evidence that checkpoint inhibitors, which have produced only modest results in breast cancer as single agents, can be far more effective in tandem with chemotherapy or other treatments.
Triple-negative breast cancer, which accounts for about 13% of breast cancer cases, is so named because it tests negative for estrogen and progesterone receptors and for the HER2 protein. Triple-negative cancers tend to grow faster than other forms of breast cancer and often carry a worse prognosis. Trials of immunotherapy agents in the disease seek to increase the treatment options available to patients.
Patients in the IMpassion031 trial were randomly assigned to receive either atezolizumab and the chemotherapy agents nab-paclitaxel, adriamycin, and cyclophosphamide, or the same chemotherapy agents plus a placebo. Their response to treatment was assessed at the time of surgery for their cancer.
“We found that the pathologic complete response rate (pCR) – the percentage of patients with no residual invasive cancer in the breast or lymph nodes at the time of surgery—was 16.5% higher in those who received atezolizumab than in those who did not,” says Elizabeth Mittendorf, MD, Ph.D., Director of the Breast Immuno-Oncology program at the Dana-Farber/Brigham and Women’s Cancer Center. Dr. Mittendorf is the principal investigator of the study. “Overall, the pCR rate was 41.1% in the chemotherapy and placebo group, compared to 57.6% in the chemotherapy and atezolizumab group.”
Intriguingly, investigators found that the improvement in pCR occurred in patients whose tumors tested negative for PD-L1 as well as those whose tumors tested positive. “This suggests that atezolizumab therapy may work for all patients undergoing treatment for early-stage triple-negative breast cancer regardless of the PD-L1 status of their tumor,” Mittendorf comments.
The incidence of serious (Grade 3 or higher) side effects was evenly balanced between the two arms of the trial, Mittendorf notes, and there were no new indications of immune-related adverse effects in patients receiving atezolizumab.
Investigators are continuing to follow the participants in the trial to determine if the pCR improvement associated with atezolizumab and chemotherapy translates into longer survival for patients, and if there are any long-term toxicities arising from the regimen.
Source: Read Full Article
