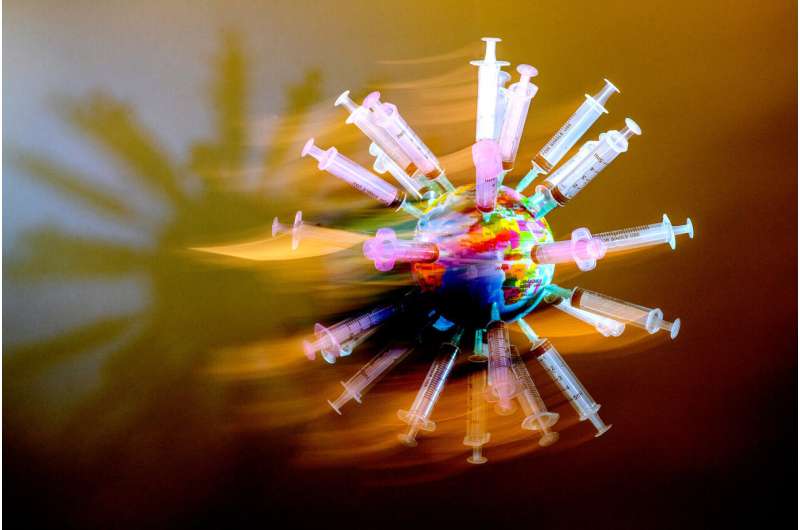
What would it take to vaccinate the world against COVID-19?
In a world of 7.9 billion people, some 5.57 billion COVID-19 vaccine doses have been administered globally. But those doses have not been distributed equally around the world. There’s a vast gulf in vaccine rates between wealthier nations and lower-income countries.
About 80% of populations in high-income and upper-middle-income countries have received a first dose, compared with only 20% of populations in low- and lower-middle-income countries, according to the World Health Organization. In just low-income countries, only 1.9% of the population has received even one dose.
At the root of that vaccine inequity, say Northeastern experts, is an issue of who is calling the metaphorical shots and why. And who is in control complicates the already difficult process of sharing the fruits of a critically important scientific enterprise: vaccine production and distribution.
“A critical element of supply chain management that people overlook is power,” says Nada Sanders, distinguished professor of supply chain management at Northeastern. “Power is an incredibly powerful force, pun not intended there.”
A program called COVAX was established by the World Health Organization and other global health organizations in an attempt to mitigate the disparity. The program leverages the financial backing of wealthier countries to distribute vaccines to people around the world. But in the past year, officials in wealthy countries bought up much of the initial supply of vaccines rather than redistribute them, in some cases to fill stockpiles for the possibility of future doses being needed.
When the White House announced that the United States would be administering a third shot to Americans starting in September, it generated ire among those watching the international vaccine rollout. Their argument: Why focus on boosting the immunity of those who already have some protection when the virus is mutating into increasingly dangerous variants as it spreads among unvaccinated communities globally?
There are generally two possible approaches to getting shots in arms around the world more readily, says Brook Baker, professor of law at Northeastern and a senior policy analyst for Health GAP (Global Access Project).
The first one, which he describes as the “status quo,” relies on drug companies to increase their capacities to manufacture vaccines and be willing to share doses to lower-income countries without increasing the prices. But for now, he says, that system is encouraging rich countries to buy up doses while the companies are largely not compelled to share with places that can’t pay as much.
The other approach, he says, would be for governments to force drug companies to share their intellectual property around COVID-19 vaccines. Essentially, they would need to share the recipe with other people who wanted to make the life-saving vaccine.
Such a knowledge-sharing approach would need to go beyond simply sharing the recipe, however, Baker says. “You need a cooking class, you need a kitchen, you need an inspector to make sure there aren’t mice and roaches running around,” he says, extending the recipe analogy.
Sanders agrees, adding that a country may not have the materials, or the technological know-how to produce the vaccines themselves.
“It’s complicated. It needs to be done in a very wise way,” Sanders says. “It also has the potential for a lot of bad actors to come in.”
There is already an illegal market for COVID-19 vaccines, as well as personal protective equipment, vaccination cards, coronavirus tests, and other certifications, says Nikos Passas, professor of criminology and criminal justice and co-director of the Institute for Security and Public Policy at Northeastern. He is also leading a study to explore ways to disrupt the flow of money in illicit and counterfeit medicine networks.
“The minute the Russians and Chinese made available their vaccines, because they came first, there were immediately sales of fake vaccines of these products on the dark web,” Passas says. The illegal market for some of the Western vaccines has been smaller, however, he says, because the vaccine is freely available from approved, official channels (like pharmacies, health clinics, and hospitals) in the U.S., for example. In countries where vaccines are in short supply or more difficult to get, he says, there is more motive for people to steal shots or create fake ones to sell.
Baker and Sanders both advocate for the creation of hubs to manufacture vaccines, located in places around the world where they could reach the most people. Such facilities would be built as training centers where the technology to manufacture the vaccines is built to an industrial scale and all of the safety controls are in place. Partners would be brought in to create a sort of apprenticeship program to establish more local know-how to produce the shots at a larger scale.
The World Health Organization and COVAX are currently working to set up such a technology transfer hub for the mRNA vaccine technologies in South Africa.
“It’s just getting off its feet. It doesn’t have the super strong financial support yet, but it’s promising,” Baker says. “Should we have started that last year? Yes. If we didn’t start last year, should we start this year? Yes.”
It’s not just about who has the technology and who has the money to pay for it, however, says Sanders. Human relationships, communication, and negotiation also play significant roles. “This is one of the reasons we do not have a ‘united world,'” she says. “Technology alone is not the answer and it is illustrated by the problems we see.”
Regardless, Baker says, the continual emergence of variants of the virus elevates the threat that the COVID-19 pandemic will continue to devastate the globe, and raises the sense of urgency to shrink the sizes of unvaccinated communities around the world.
Source: Read Full Article
