singulair causing depression and suicide
The number of mass shooting incidents (MSI) has been increasing in recent years, rising nearly 40 percent from 2019 to 2021. Although research has been done to identify ways to prevent mass shootings and reduce death and injury, there have not been specific details about the medical system response to such events, according to study authors who recently published their findings as an “article in press” in the Journal of the American College of Surgeons.
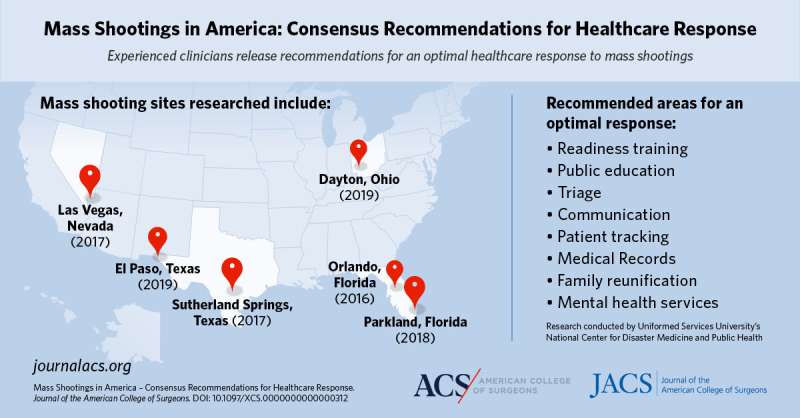
Uniformed Services University’s National Center for Disaster Medicine and Public Health hosted a consensus conference in September 2021 to bring together clinicians from six sites where mass shootings occurred and more than 15 people were killed or injured. These locations were in Orlando, cheap vytorin au no prescription Fla. (2016); Las Vegas, Nev. (2017); Sutherland Springs, Texas (2017); Parkland, Fla. (2018); El Paso, Texas (2019); and Dayton, Ohio (2019). The recommendations from the conference will help healthcare facilities better respond when a mass shooting occurs nearby.
“We recognized that mass shootings are frequent events that occur in the United States and wondered if we could learn more about how to optimize response to these incidents,” said lead study author Craig Goolsby, MD, MEd, FACEP, a professor and the vice chair of USU’s Department of Military and Emergency Medicine, and the science director of the National Center for Disaster Medicine and Public Health. “We identified a group of recent mass shootings and then invited clinicians who participated in the healthcare response—EMS clinicians, emergency physicians, and surgeons—to participate in our conference.”
Convening expert clinicians
After completing a two-part pre-conference survey, representatives from each site gave a presentation about their activities and experience during their response to the mass shooting. The study team generated 12 common themes from the survey responses and presentations: prior training; exercises; readiness; community preparation of bystanders, civilians, and law enforcement; triage; communications; patient identification and tracking; space expansion plans; staffing; military-civilian collaboration; clinical treatment best practices; medical records (documentation); family reunification; and grieving and after-action mental health.
The final day of the conference consisted of breaking into subgroups based on expertise (EMS, emergency medicine, and surgery). Each subgroup was asked to create specific recommendations for each of the themes identified by the study team, and to generate any additional themes that the subgroups thought were missing. The emergency medicine and surgery groups did not add any other themes, and the EMS group added unified command, scene management, and EMS to hospital assistance.
Recommendations for healthcare response
After the conference, two of the study authors reviewed each group’s consensus statements to identify common themes. Through this review, the authors identified eight recommendations that were similar across all three groups:
- Readiness training: Regular, multi-domain training activities, which mirror the realism of actual events, to ensure readiness of the entire community system.
- Public education: Prior public education or immediate direction from web-based mapping programs about the appropriate hospitals to bring MSI patients for care.
- Triage: A staged and iterative triage process at the scene, emergency department, and to prioritize operative care.
- Communication: Effective communication between prehospital personnel at the scene and hospitals.
- Patient tracking: A patient tracking system that functions from point-of-injury through all subsequent healthcare.
- Medical Records: Rehearsal with and rapid availability of alternative methods of patient care documentation and order entry.
- Family reunification: Rapid implementation of organized, well-communicated family reunification and assistance services.
- Mental health services: Tailored after-action mental health services for responding professionals.
https://youtube.com/watch?v=9WU40UApmtA%3Fcolor%3Dwhite
Dr. Goolsby noted that many of these recommendations can be implemented fairly easily. A recommendation he thought was particularly important was a modified triage plan for mass shooting patients.
“The participants identified that for shootings, looking at anatomic considerations—where the bullet holes are on a patient—is really important in getting them to the right care as quickly as possible,” said Dr. Goolsby. “That could be a pretty easy recommendation for hospitals to implement.”
Getting patients the right care after a mass shooting
These recommendations can help any healthcare facility better respond if a mass shooting occurs nearby. However, preparing for a mass shooting and addressing firearm violence that happens on a daily basis require different plans to best care for patients. Study coauthor Deborah A. Kuhls, MD, FACS, FCCM, assistant dean for research and professor of surgery, Kirk Kerkorian School of Medicine, University of Nevada, Las Vegas, who was part of the response to the 2017 mass shooting in Las Vegas, said that while mass shootings make up a small percentage of the deaths occurring each year from firearms in the United States, they are horrific events. The more common causes of death and injury from firearms are individual homicides and suicides. But when a mass shooting occurs, it requires a different healthcare response to effectively care for the patients.
“What is really different is that with one gunshot wound patient coming in, I focus my attention on that patient. In a mass casualty event, there is a large number of people who appear at once and we have to decide who needs our attention the most, who has the greatest threat to life,” said Dr. Kuhls.
She also noted that by properly triaging patients in a mass shooting incident, those with more severe injuries can be treated at a trauma center and those with less severe injuries can be treated at a non-trauma center. This helps ensure trauma centers don’t become overwhelmed and each patient is able to get the level of care they need.
Importance of STOP THE BLEED
The focus of the conference and recommendations was how healthcare clinicians and organizations, from point of injury to the hospital, can best respond once victims are injured in a mass shooting. Dr. Goolsby and Dr. Kuhls stressed the importance of prehospital care, such as training the pubic in bleeding control techniques through the STOP THE BLEED program. Bleeding control training for the public came up during the conference as a way for the public to help save lives in a mass shooting situation.
“A number of participants in the conference talked about how patients arrived with tourniquets in place that they thought were probably lifesaving,” Dr. Goolsby said.
Source: Read Full Article
